
Explore This Issue
ACEP Now: Vol 41 – No 01 – January 2022The Case
The trauma radio alert advises EMS is five minutes out with a patient with gunshot wounds to the head. The patient was reportedly shot in the head after he attacked a state trooper during a traffic stop on the interstate. The paramedic reports that the patient has two head wounds, is orally intubated, is tachycardic at 120, has a blood pressure of 136/92, and has a Glasgow Coma Score (GCS) of 7T.
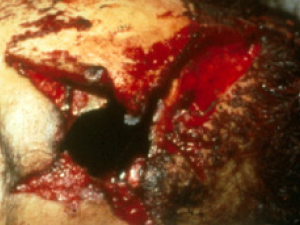
Prior to the patient’s arrival, you notice multiple police officers arriving and standing outside of the resuscitation room door. One of the commanding officers walks up to you and says, “Doc, we think the suspect tackled the trooper, strangled her, and tried to take her gun when he was shot. Can you please take a close look at the wounds and let us know which wound is the entrance, which wound is the exit, and how far away the gun was from the suspect’s head when he was shot by our female trooper?” When the patient arrives in the resuscitation room, you observe a large wound on the right temple (see Photo 1) and a smaller wound on the left parietal area (see Photo 2). After your initial and secondary assessments, you consult trauma and neurosurgery and send the stable patient to radiology for a CT scan of his head and cervical spine. As you leave the resuscitation room, the commanding officer again approaches you and says, “Doc, given the current political environment of officer-involved shootings in the country, it is critical that we know which wound is the entrance, which is the exit, and how far away the trooper’s gun was from the suspect when he was shot. Doc, what did you document in the chart, and what do you think about the wounds?”
Table 1: The six common physical characteristics of entrance wounds and their causes
| Abrasion Collar caused by friction with the bullet |
| Tattooing caused by unburned gunpowder |
| Soot caused by the residue of burned gunpowder |
| Seared Skin caused by the flame and hot gases |
| Triangular Tears caused by skin expansion from injected gas |
| Muzzle Contusion caused from injected gases pushing expanding skin against barrel |
Based on your visual assessment of the wounds, how will you answer the following questions that will be asked of you by a local prosecutor when this case of an officer-involved shooting is presented to a grand jury? The patient survived his transcranial wounds and is now a GCS 6T in a long-term care facility.
The Questions:
- What were the physical characteristics of each of the wounds you observed on the suspect’s scalp?
- Which wound was the entrance wound?
- How did you determine which wound was the entrance wound?
- Which wound was the exit wound?
- How far was the trooper’s gun from the suspect’s head when he was shot by the trooper?
- If the trooper said she placed her gun against the suspect’s scalp as she was about to go unconscious from being strangled by the suspect, are the injuries consistent with her statements?
Clinical Forensic Medicine and Gunshot Wounds
Patients who are victims of gun violence present to the emergency department with both medical needs and forensic issues. The patient is part of the crime scene, all evidence of which is only seconds away from being inevitably and irretrievably washed or debrided away. In these fleeting moments, both health and justice are held in the physician’s hands. Unless you have had advanced forensic training, you are not the forensic expert. What you document is for others to interpret. To prevent a miscarriage of justice and preserve the evidence, all you must do is describe what you find.
Since a picture is worth a thousand words, the easiest way to “describe” and document the injuries and the evidence is with a camera. Make sure that your department has one and that it is capable of close-up photographs. Some electronic medical record systems permit you to take HIPAA-compliant photographs with your own cellphone and import these into the patient’s chart.
The purpose of this article is to give emergency physicians a simple list of gunshot wound characteristics to photograph or, in the absence of photographic documentation, to describe. Table 1 lists these physical characteristics and contains recognized terms utilized by forensic physicians around the world.
The Physical Characteristics of Entrance Wounds from Handguns
The physical characteristics of an entrance wound depend primarily on two factors: 1) the range of fire (the distance from the muzzle to the skin) and 2) the presence of any intermediate objects (eg, clothing, glass). Range of fire is divided into four general categories: distant (or indeterminate), intermediate, close, and contact (see Table 2). Each range of fire is associated with specific wound characteristics:
- Distant- or indeterminate-range wounds have only an abrasion collar (see Photos 3 and 4).
- Intermediate-range wounds have an abrasion collar and tattooing or stippling (see Photo 5).
- Close-range wounds have an abrasion collar, soot, and tattooing (see Photo 6).
- Contact wounds have soot, seared skin, and triangular-shaped tears (see Photo 7).
Distant-Range Wounds: Only the bullet contacts the skin in a distant- or indeterminate-range wound. When a bullet penetrates skin, there is friction between the projectile and the epithelial tissue, which creates an abrasion collar (see Photo 3 and Figure 1). Abrasion collars will vary in appearance depending on the angle of penetration (see Photo 4 and Figure 2). All entrance wounds will have some degree of an abrasion collar, with the exception of those wounds to the palms of the hands and soles of the feet, where the epithelium is highly keratinized. Abrasion collars may also be referred to as an abrasion margin, abrasion rim, or abrasion ring.
Intermediate-Range Wounds: These are characterized by the presence of an abrasion collar plus the presence of punctate abrasions referred to as tattooing or stippling (see Photo 5). The punctate abrasions occur when unburned or partially burned pieces of gunpowder impact the skin. Tattooing on the skin may be visualized from distances as close as 0.5 inches or as far away as 48 inches. The density and pattern of the punctate abrasions will vary depending on the muzzle-to-skin distance, the length of the gun barrel, the presence of intermediate objects, and the amount of gunpowder within a particular cartridge.
Close-Range Wounds: Close-range wounds are defined as the range at which the carbonatous residue of combustion, or soot, is visible surrounding the wound or on clothing (see Photo 6). The presence of soot may cover and obscure the abrasion collar. Soot is short-lived evidence and can easily be washed away during emergency care and treatment.
Contact Wounds: A contact wound is one in which the barrel is in contact with the victim’s clothing or skin. Because contact entrance wounds can vary in appearance from small to very large depending on the elasticity of the skin and the volume of gas injected, they are frequently misinterpreted as exit wounds (see Photos 1 and 7). A contact wound to the temple from a .22-caliber short cartridge will appear as a small hole with seared blackened edges and only tiny triangle-shaped tears (see Photo 8), while a contact wound to the forehead from a .357-caliber Magnum load will create a large defect (see Photo 9). The large volume of gas injected into scalp tissue from a Magnum load will expand the tissue, resulting in a large, gaping wound. Note the characteristic stellate pattern caused by the ripping and tearing of the skin. Because these wounds are so large and are frequently misinterpreted as exit wounds, remember that the size of the wound is not used to determine entrance or exit. Close examination of the wound margins of all contact wounds will reveal the presence of soot. Also, there will be seared skin from the discharge of hot gases and an actual flame that extends from the gun barrel.
The injection of gases into tissue can cause the skin to expand against the barrel or muzzle of the handgun with sufficient force to impart a contusion that mirrors the pattern of the barrel. This imprint is called a muzzle contusion or muzzle abrasion and may provide forensic investigators with critical information on the characteristics of the weapon’s barrel: revolver versus semiautomatic handgun (see Photo 10).

Photo 2: Wound on the patient’s left parietal scalp.

Photo 3: Distant wound with an abrasion collar.

Photo 4: Comet-tailed abrasion collar (12 to 6 o’clock position) from a bullet’s angled entry.

Photo 5: Intermediate-range wound with an abrasion collar and more than 100 punctate abrasions, or tattooing, from unburned pieces of gunpowder impacting the skin.

Figure 1: An abrasion collar is created from friction between the bullet and the skin (see Photo 3).
ILLUSTRATIONS: Yesenia Aceves

Figure 2: An angled, or comet-tailed, abrasion collar from an angled entry (see Photo 4).
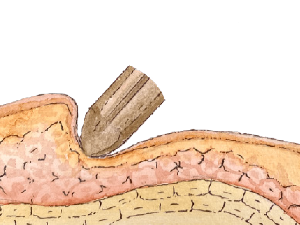
Figure 3: An angled, or comet-tailed, abrasion collar from an angled entry (see Photo 4).
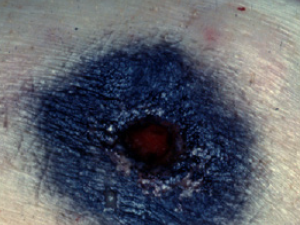
Photo 6: Close-range wound with soot.
PHOTOS: Bill Smock

Photo 8: Contact wound with soot, seared skin, and small triangular-shaped tears from a .22-caliber pistol.

Photo 7: Contact wound with soot, seared skin, and triangular-shaped tears.
tears from a .357 Magnum pistol.
Conclusion
Emergency physicians are in an ideal position to evaluate and document the state of a gunshot wound because they see and explore it before it is disturbed, distorted, or destroyed by treatment or surgical intervention. Documentation of gunshot wounds should always include the anatomical location, size, shape, and distinguishing forensic characteristics (see Table 1). Emergency clinicians, unless they have specialized forensic training, should never describe wounds as “entrance” or “exit.” Exit wounds are not always larger than their associated entrance wound. Wound size does not even consistently correspond to bullet caliber. Wounds can expand or contract depending on tissue elasticity and the presence or absence of hemorrhage.

Photo 10: Contact wound with soot, seared skin, triangular-shaped tears, and a muzzle contusion from a .32-caliber pistol.
Table 2: Range of fire as determined by wound characteristics.
| Distance | Appearance |
|---|---|
| Contact: Tight or loose |
Seared skin, triangle-shaped tears, soot |
| Close: 0–6” |
Soot, tattooing and abrasion collar |
| Intermediate: up to 48” |
“tattooing” and abrasion collar |
| Distant or indeterminate | Abrasion collar |
Some emergency departments use forensic nurse examiners to address the forensic needs of their living patients. Forensic nurse examiners can photograph and diagram a patient’s wounds and, with sufficient forensic training, can determine whether the injuries observed are consistent with the history reported. Such forensic nursing services clearly benefit the forensic needs of emergency departments and their patients. They also free doctors to focus on practicing medicine and help keep emergency physicians from uncompensated trips to court.
Note: The grand jury questions and the evaluation of exit wounds will be answered in a future issue.
Acknowledgements: Thank you to Yesenia Aceves for the beautiful watercolor illustrations.
 Dr. Smock is the full-time police surgeon for the Louisville Metro Police Department and a clinical professor of emergency medicine at the University of Louisville School of Medicine in Kentucky.
Dr. Smock is the full-time police surgeon for the Louisville Metro Police Department and a clinical professor of emergency medicine at the University of Louisville School of Medicine in Kentucky.




One Response to “The Clinical Forensic Evaluation of Gunshot Wounds in the ED”
March 22, 2023
BeverlyThank you. This really helps me understand my son’s gunshot wound very informative..