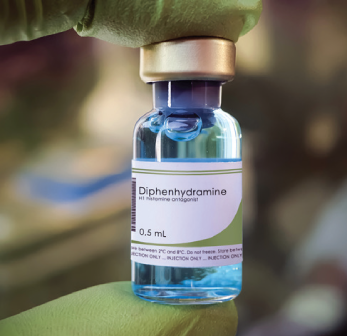
Diphenhydramine (Benadryl), is ubiquitous in the emergency department (ED) and has historically been a component of many treatment algorithms. Urticaria? Take some diphenhydramine. Allergic reaction or anaphylaxis? Give them diphenhydramine. Migraine? Let’s add some diphenhydramine to the mix. Yet, there is essentially no reason to administer diphenhydramine to ED patients. Alternatives to diphenhydramine exist that are less sedating, possess fewer anticholinergic effects, and are equally efficacious. In fact, many professional society guidelines have urged emergency physicians to stop using diphenhydramine for years.
Explore This Issue
ACEP Now: Vol 41 – No 07 – July 2022Not-So-Commonly Known Side Effects
Diphenhydramine is the most popular first-generation antihistamine in the United States—a medicine cabinet staple—probably because it has been around for over 70 years. However, many suggest that the medication would not be approved today as an over-the-counter medication. There are significant safety concerns regarding diphenhydramine. As a first-generation antihistamine, diphenhydramine readily crosses the blood-brain barrier. As a result, it is associated with sleepiness, even persisting the morning after a single evening dose. Its sedative effects throughout the central nervous system can last longer than 12 hours, far beyond its therapeutic actions. Sleepiness alone, however, isn’t the only side effect. This class of antihistamines that diphenhydramine is associated with cause impaired cognition and psychomotor performance, including during driving, and has been linked to accidental injury.1 One randomized trial found that a dose of diphenhydramine was associated with markers of impaired driving worse than a blood alcohol concentration of roughly 0.1 percent.2
In addition to the cognitive side effects, first-generation antihistamines have poor selectivity to the brain’s H1 histamine receptors and can result in heightened anticholinergic and antimuscarinic responses. Older patients are particularly at risk of cognitive decline and other adverse effects.3 In addition to these adverse events, diphenhydramine is abused by some to generate hallucinations or a sensation of being “high” (particularly associated with rapid intravenous administration).
Alternatives, like second- and third-generation antihistamines, offer more favorable risk-benefit profiles. These medications less readily cross the blood-brain barrier, translating to less sedation, less cognitive impairment, and less potential for abuse. Oral second-generation antihistamines such as cetirizine, fexofenadine, and levocetirizine work at least as fast as diphenhydramine.1
Allergic Reactions and Anaphylaxis
Of the indications for diphenhydramine, immediate hypersensitivity reactions such as allergic conditions and anaphylaxis may seem obvious. Yet, a 2020 practice statement from the American Academy of Allergy Asthma, and Immunology (AAAAI) recommends against the administration of any antihistamine in the acute phase of anaphylaxis or for the prevention of biphasic reactions.4 Indeed, the treatment for anaphylaxis is epinephrine and antihistamines do not have life-saving effects in this disease process. The practice update states that antihistamines may be used as adjuncts but, in this case, they advocate for the use of second-generation H1-blockers. One argument for the continued use of diphenhydramine is the ability to administer the medication intravenously or intramuscularly. However, diphenhydramine does not need to be given emergently in anaphylaxis or allergic reactions. It is an adjunct, an aid for symptomatic control and, as such it can be given orally after epinephrine has stabilized the patient.
Pages: 1 2 3 | Single Page





6 Responses to “The Death of Diphenhydramine”
July 17, 2022
Michael BernsteinI am in agreement with almost all of this. However, and strictly from personal and anecdotal experience, I still feel it is efficacious as an adjunct in the “migraine cocktail”. I use 12.5 mg IV (with Regaln and Toradol) in those with significant nausea, as I think it’s antiemetic properties help. Additionally, I think it’s sedative properties help in the agitated patient that I am giving Haldol and Ativan to. I am trying to switch to atypical antipsychotics or Ketamine when I can, but still occasionally reach for the old B52 if it’s my only choice. I guess now, with the lack of availability of Ativan it would be B55 with Midazolam….In these two instances I feel that the risk/benefit profile favors the potential benefit.
July 17, 2022
Charlene DoyleRegarding benadryl for migraine – sleep is usually the true treatment for migraine. Unfortunately it is difficult to achieve with a migraine but quite easy with benadryl. Also, who has access to droperidol, one of my favorite medications.
July 17, 2022
Misty Navarro GreensonI have been adding 12.5 mg of Benadryl to my migraine cocktail for 20 years and have never had any issues. I don’t have a lot of patients with akisthesia and when I have an extra 12.5 has relieved these symptoms. I don’t see the evidence for this sweeping statement. Please educate me.
September 1, 2022
Louise B AndrewI too would never bury Benadryl. I well remember our collective professional relief when the Phenergan-Reglan-Benadryl cocktail freed us from having to use narcotics for migraines… and it had about a 99% success rate. The Benadryl probably prevented dystonic reactions, and if it caused drowsiness, well, YES, that helps greatly to break the cycle of a migraine. As a migraineur, I used this on myself (not on duty of course) and just don’t believe this is any less safe than any of the other formulations mentioned.
What are you doing for dystonic reactions incidentally? Some expensive new drug?
September 4, 2022
JSWBenadryl isn’t going anywhere. Because I can’t remember the last time is caused any serious adverse effects clinically in the ED. Cool story though.
September 10, 2022
W. Anthony GerardThank you, Dr. Westhafer for this interesting article. I think you appropriately challenge all of us to be cautious when we use Diphenhydramine.
But maybe your title, and your premise, should be asked as a question, instead of stated as an imperative? ( Ie, Is this the Death of Diphenhydramine?)
I agree with the other physicians who commented above. I would like to see evidence, or a more detailed discussion, of the use of Benadryl for migraines in combination with Compazine.
How about as a local anesthetic when pts are allergic to lidocaine? There are other indications for this medication that weren’t discussed, and should be, before we drop it’s use.
Finally, I don’t think you looked at the evidence suggesting that sedation could be a benefit, rather than risk, in many patients with urticaria and pruritis?
Second and third generation antihistamines work rapidly and have less sedation, but there is still an indication for First generation antihistamines ( diphenhydramine) in patients who with “severe” pruritis – at least q hs.
There is an evidence-based review of the efficacy of antihistamines in relieving pruritus from atopic dermatitis ( AT) published in Arch Dermatol 1999;135:1522–5. It’s been challenged recently by other studies of AT.
I don’t know of any evidence outside the derm literature comparing First and Second generation anti-histamines for other causes of pruritis, but I still use Bendadryl for severe itching in patients with pruritis at least at bedtime. And that’s what I’m taking if I ever get severe
rhus dermatitis.
Maybe one of our EBM or pharmacology colleagues can give us more information about these issue in a follow -up article?