Risk Versus Reward
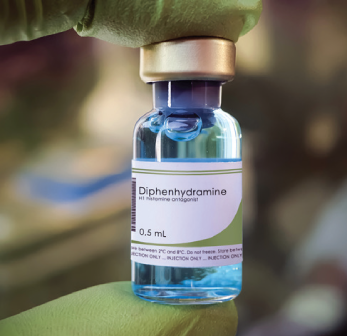
Diphenhydramine has an unfavorable risk-benefit profile. For nearly every indication, a less risky alternative exists. It remains unclear why, despite the mountain of evidence that we should not use diphenhydramine, this medication remains one of the most commonly used antihistamines. It is time to get with the guidelines and drop diphenhydramine, for nearly any indication, and encourage our patients to do the same.
Explore This Issue
ACEP Now: Vol 41 – No 07 – July 2022Dr. Westafer (@LWestafer) is assistant professor of emergency medicine and emergency medicine research fellowship director at the University of Massachusetts Medical School–Baystate and co-host of FOAMcast.
References
- Fein MN, Fischer DA, O’Keefe AW, et al. CSACI position statement: Newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for the treatment of allergic rhinitis and urticaria. Allergy Asthma Clin Immunol. 2019;15:61.
- Weiler JM, Bloomfield JR, Woodworth GG, et al. Effects of fexofenadine, diphenhydramine, and alcohol on driving performance. A randomized, placebo-controlled trial in the Iowa driving simulator. Ann Intern Med. 2000;132(5):354–363.
- Agostini JV, Leo-Summers LS, Inouye SK. Cognitive and other adverse effects of diphenhydramine use in hospitalized older patients. Arch Intern Med. 2001;161(17):2091–2097.
- Shaker MS, Wallace DV, Golden DBK, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol. 2020;145(4):1082–1123.
- Grattan C, Powell S, Humphreys F, et al. Management and diagnostic guidelines for urticaria and angiooedema. Br J Dermatol. 2001;144(4):708–714.
- Zuberbier T, Asero R, Bindslev-Jensen C, et al. EAACI/GA(2)LEN/EDF/WAO guideline: management of urticaria. Allergy. 2009;64(10):1427–1443.
- Zuberbier T, Abdul Latiff AH, Abuzakouk M, et al. The international EAACI/GA2LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy. 2022;77(3):734–766.
- Friedman BW, Cabral L, Adewunmi V, et al. Diphenhydramine as Adjuvant Therapy for Acute Migraine: An Emergency Department-Based Randomized Clinical Trial. Ann Emerg Med. 2015;67(1):32–39.e3.
- Vinson DR, Drotts DL. Diphenhydramine for the prevention of akathisia induced by prochlorperazine: a randomized, controlled trial. Ann Emerg Med. 2001;37(2):125–131.
- Church MK, Maurer M, Simons FER, et al. Risk of first-generation H(1)-antihistamines: a GA(2)LEN position paper. Allergy. 2010;65(4):459–466.
Pages: 1 2 3 | Single Page





6 Responses to “The Death of Diphenhydramine”
July 17, 2022
Michael BernsteinI am in agreement with almost all of this. However, and strictly from personal and anecdotal experience, I still feel it is efficacious as an adjunct in the “migraine cocktail”. I use 12.5 mg IV (with Regaln and Toradol) in those with significant nausea, as I think it’s antiemetic properties help. Additionally, I think it’s sedative properties help in the agitated patient that I am giving Haldol and Ativan to. I am trying to switch to atypical antipsychotics or Ketamine when I can, but still occasionally reach for the old B52 if it’s my only choice. I guess now, with the lack of availability of Ativan it would be B55 with Midazolam….In these two instances I feel that the risk/benefit profile favors the potential benefit.
July 17, 2022
Charlene DoyleRegarding benadryl for migraine – sleep is usually the true treatment for migraine. Unfortunately it is difficult to achieve with a migraine but quite easy with benadryl. Also, who has access to droperidol, one of my favorite medications.
July 17, 2022
Misty Navarro GreensonI have been adding 12.5 mg of Benadryl to my migraine cocktail for 20 years and have never had any issues. I don’t have a lot of patients with akisthesia and when I have an extra 12.5 has relieved these symptoms. I don’t see the evidence for this sweeping statement. Please educate me.
September 1, 2022
Louise B AndrewI too would never bury Benadryl. I well remember our collective professional relief when the Phenergan-Reglan-Benadryl cocktail freed us from having to use narcotics for migraines… and it had about a 99% success rate. The Benadryl probably prevented dystonic reactions, and if it caused drowsiness, well, YES, that helps greatly to break the cycle of a migraine. As a migraineur, I used this on myself (not on duty of course) and just don’t believe this is any less safe than any of the other formulations mentioned.
What are you doing for dystonic reactions incidentally? Some expensive new drug?
September 4, 2022
JSWBenadryl isn’t going anywhere. Because I can’t remember the last time is caused any serious adverse effects clinically in the ED. Cool story though.
September 10, 2022
W. Anthony GerardThank you, Dr. Westhafer for this interesting article. I think you appropriately challenge all of us to be cautious when we use Diphenhydramine.
But maybe your title, and your premise, should be asked as a question, instead of stated as an imperative? ( Ie, Is this the Death of Diphenhydramine?)
I agree with the other physicians who commented above. I would like to see evidence, or a more detailed discussion, of the use of Benadryl for migraines in combination with Compazine.
How about as a local anesthetic when pts are allergic to lidocaine? There are other indications for this medication that weren’t discussed, and should be, before we drop it’s use.
Finally, I don’t think you looked at the evidence suggesting that sedation could be a benefit, rather than risk, in many patients with urticaria and pruritis?
Second and third generation antihistamines work rapidly and have less sedation, but there is still an indication for First generation antihistamines ( diphenhydramine) in patients who with “severe” pruritis – at least q hs.
There is an evidence-based review of the efficacy of antihistamines in relieving pruritus from atopic dermatitis ( AT) published in Arch Dermatol 1999;135:1522–5. It’s been challenged recently by other studies of AT.
I don’t know of any evidence outside the derm literature comparing First and Second generation anti-histamines for other causes of pruritis, but I still use Bendadryl for severe itching in patients with pruritis at least at bedtime. And that’s what I’m taking if I ever get severe
rhus dermatitis.
Maybe one of our EBM or pharmacology colleagues can give us more information about these issue in a follow -up article?