The NM Bridge Process
Engaged hospitals were eligible for one year of funding to support the hospital and clinicians in establishing ED-based MOUD programs. Funding covered clinical time, educational opportunities, and trainings. One year of salary was available for a peer-support worker or social worker to link the patient to treatment in the community, improving follow-up.8
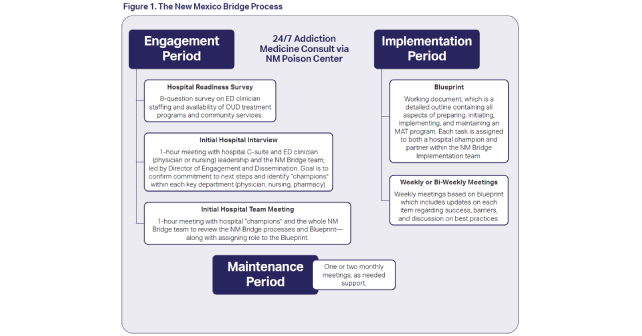
The NM Bridge process has three stages: engagement, implementation, and maintenance periods (Figure 1). Engagement focuses on initial outreach and confirmation of a hospital’s commitment to the program. Engaged hospitals demonstrate their commitment by completing an initial survey to identify current resources and gaps in care, assembling a team of champions including representatives from emergency physicians, nursing, social work, pharmacy, inpatient, and outpatient (Table 2), and submitting a budget to the Behavioral Health Service Division. In the implementation period, the implementation team and the hospital’s champions meet weekly, aligning their work to the NM Bridge’s blueprint (Table 3). During the maintenance phase, meetings typically move to once monthly, with the option to meet more often as needed to address any issues as they arise.
Addressing Rural Disparities
The NM Bridge is designed to increase the number of prescribers and hospital staff who can treat OUD, increasing access to these services in rural New Mexico. Rural communities in NM face the highest rates of OUD overdose, which is increasingly impacting indigenous communities and rates are disproportionately high among the American Indian/Alaska Native (AI/AN).3,9 Implementing MOUD programs at rural hospitals is challenging due to limited workforce, a lack of dedicated personnel for quality improvement, thin financial margins, and OUD-related stigma. NM Bridge addresses all of these barriers by supporting rural hospitals with a dedicated team using a hands-on approach of MOUD implementation with financial support and robust training.
Grant support is key and brings needed resources to rural hospitals. This includes the implementation team’s expertise, along with financing to hire a peer-support position or a social worker and to cover clinician and staff education time. Trainings address stigma and education across all clinician groups and are designed for the rural context. Through weekly meetings and hands-on partnership, the implementation team directly facilitates the local hospital’s implementation. As the rural outpatient ecosystem is fragile, a critical aspect of the program is assuring continued MOUD following ED or hospital discharge. The clinic/outpatient champion role is designed to address this rural-specific consideration by confirming outpatient follow-up. Further, hospitals identify a backup, community-based, OUD treatment program, and at minimum establish a relationship with a telemedicine service.
Pages: 1 2 3 4 | Single Page






No Responses to “The New Mexico Bridge Program”