“Time is myocardium.” Emergency, prehospital, and regional systems have been built around this slogan and are designed to get patients with acute myocardial infarctions, specifically ST-elevation myocardial infarctions (STEMIs), early reperfusion therapy. The American College of Cardiology (ACC) has now caught up with the addition of four “STEMI equivalents,” meaning many more patients should receive cardiac catherization or other means of reperfusion based on more subtle electrocardiogram (ECG) changes.
Explore This Issue
ACEP Now: Vol 41 – No 12 – December 2022How did we get here?
The 2013 American Heart Association (AHA) 2013 guidelines defined STEMI in a rudimentary fashion. Patients with the clinical syndrome fitting with acute coronary syndrome (ACS) must also have at least one of the following (in the absence of left ventricular hypertrophy or left bundle-branch block [LBBB]) on ECG:
- New ST elevation at the J point in at least 2 contiguous leads of ≥2 mm in men or ≥1.5 mm in women in leads V2–V3
- ≥1 mm (0.1 mV) in other contiguous chest leads or the limb leads1
At that time, the guidelines referred to proposed criteria for recognizing ischemia in the presence of an LBBB but did not endorse the Sgarbossa criteria.
Some have argued for years, however, that the STEMI versus non-STEMI dichotomy should be abandoned in favor of targeting occlusion myocardial infarctions (OMIs) for reperfusion therapy, some of which may not meet the ECG definition of STEMI.2,3,4 The most recent consensus statement from the ACC nudges towards recognizing OMI by recommending that four “STEMI equivalents” be treated according to routine STEMI protocols. In fact, the statement highlights the importance of this shift by stating, “the application of STEMI ECG criteria on a standard 12-lead ECG alone will miss a significant minority of patients who have acute coronary occlusion.”5 While the guidelines don’t replace “STEMI” with an inclusive term for those who would benefit from emergent reperfusion therapy, they take a step towards emphasizing that time is myocardium by including ECG patterns indicating early coronary occlusion.
Activate the cath lab or reperfusion treatment for these four ECG patterns
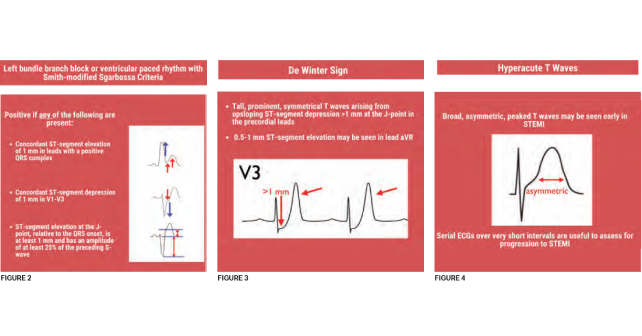
Patients who should be managed as a STEMI and receive early reperfusion therapy are those with traditional STEMI as well as those with one of the following STEMI equivalents: posterior STEMI, LBBB with Sgarbossa or Smith-modified Sgarbossa criteria, DeWinter sign, or hyperacute T waves. The first two STEMI equivalents are unsurprising and have probably triggered cardiac catheterization lab activations across the United States for years. However, the latter STEMI equivalents have only more recently gained recognition.
Pages: 1 2 3 4 | Single Page




One Response to “The Reperfusion Guidelines Finally Catch Up”
December 21, 2022
Scott R CentersFantastic synopsis and education around STEMI equivalents. I was preparing an educational update for my team when this popped up in my inbox. Dr. Westafer did a much better and more thorough job than I could have.
Kudos and thanks,
Scott R. Centers, MD
Medical Director, Emergency Services
Caromont Health
Gastonia, NC