
Post-arrest patients with more significant reperfusion injury (for example, Pittsburgh Cardiac Arrest Category (PCAC) greater than or equal to 3, revised post-Cardiac Arrest Syndrome for Therapeutic hypothermia score (rCAST) greater than 6, evidence of shock, and/or longer arrest times) may benefit from mild hypothermia to 33 degrees Celsius, while less severe post-arrest patients may benefit from fever prevention at less than 37.5 degrees Celsius.
Explore This Issue
ACEP Now: Vol 43 – No 04 – April 2024How Did We Get Here?
Targeted temperature management (TTM) for patients following cardiac arrest resuscitation has gone through several dosing iterations in the past two decades. Early work on TTM in 2002 showed benefit to cooling to 33 degrees Celsius, which subsequently influenced international resuscitation guidelines to recommend mild hypothermia at 32 degrees to 34 degrees Celsius in 2005.1,2 However, the European TTM1 trial in 2013 showed similar outcomes for those cooled to 33 degrees Celsius compared to 36 degrees Celsius, leading to a 2015 AHA class I recommendation of “cooling between 32 degrees Celsius-36 degrees Celsius.”3,4 The Hyperion trial in 2019 demonstrated that TTM at 33 degrees Celsius was efficacious for non-shockable rhythms, reinforcing the guidelines recommendation for post-arrest TTM.5,6
In 2021, the TTM2 trial was published. TTM2 was a multicenter, randomized trial that enrolled 1850 OHCA patients and randomized them to 33 degrees Celsius or normothermia. Patients were maintained at their assigned target temperatures for 28 hours and then maintained at normothermia less than 37.5 degrees Celsius for 72 hours. Outcomes, including survival at 6 months and neurologic outcome, between the two groups were not clinically or statistically different, but the hypothermia group had a higher incidence of hemodynamically compromising arrythmias (24 percent versus 17 percent in the normothermia group; RR 1.45 (1.21–1.75).
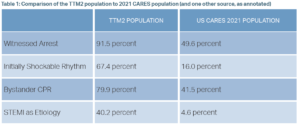
The TTM2 trial, while rigorously performed, has important limitations to generalizability for the US patient population. TTM2 primarily enrolled patients in Northern Europe and thus had a number of characteristics not seen in the U.S. As seen in Table 1, the TTM2 population had markedly more favorable prevalence of positive prognosticators of arrest, compared to an American population from the same year.7 TTM2 is generally interpreted as favoring normothermia for post-arrest care, but the question is whether this trial is broadly applicable to many countries with less developed community CPR involvement.
Current International Resuscitation Recommendations
In August 2023, the American Heart Association and the International Liaison Committee on Resuscitation published a scientific advisory that derived three conclusions.8,9 First, based on TTM2, they recommend that cooling OHCA patients of cardiac or unknown cause, excluding those with unwitnessed asystole, to less than 37.5 degrees Celsius “is a reasonable and evidence-based approach.” Second, as TTM2 did not address in-hospital cardiac arrest or OHCA of noncardiac (other medical) cause, the guidelines remain essentially equivocal as to “whether some of these patients might benefit from temperature control at temperatures between 33 degrees C and 37.5 degrees C.” Finally, the guidelines support active temperature management’s (though not necessarily hypothermia) role in improving post-arrest outcomes. This is best demonstrated by the TTM2 data showing that 46 percent of patients in the normothermia group required active cooling, on top of pharmacological antipyresis.
Pages: 1 2 3 4 | Single Page




No Responses to “The Science on Targeted Temperature Management”