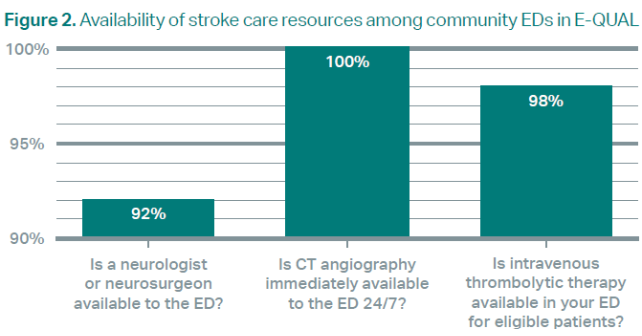
Today, the integrated stroke system of care is far advanced from when the initial research in this space was performed. We are equipped to rapidly identify eligible patients and, in most cases, have the ability to make specialist-supported treatment decisions. In fact, although they may not have an official stroke certification, data from E-QUAL showed that many U.S. hospitals are already well equipped to function as Acute Stroke Ready Hospitals. These sites have the necessary structure to receive patients with acute ischemic stroke, administer timely thrombolytics, and identify those who require transfer for thrombectomy or a higher level of care. In areas where stroke center certification does not provide a prehospital triage advantage, such as remote and rural settings, hospitals may not invest in these official designations. Nevertheless, these sites are increasingly demonstrating that they have the necessary structures to function as an Acute Stroke Ready Hospital with the right processes and resources in place.
Explore This Issue
ACEP Now: Vol 43 – No 12 – December 2024Stroke Identification
Second, emergency physicians have a broad skillset and are particularly suited for identification of patients who will benefit from all types of treatments—from extracorporeal membrane oxygenation to lithotripsy. We combine data related to the patient’s profile, physical examination, onset of timing, and imaging results to form the complete clinical picture. Our role is no longer to decide whether thrombolytics work or not, but to identify and treat patients who will benefit. The latest research underscored that there is more nuance to treatment than a simple “yes” or “no” for thrombolytics, and that our skillset, along with our consultants, can help drive the best outcomes for our patients.4
For example, in the prehospital setting, we must consider how potential stroke is identified and which patients should be diverted to thrombectomy-capable and comprehensive stroke centers to ensure timely treatments, while avoiding overwhelming already-full tertiary care centers. In the ED, how do we create efficient and effective stroke protocols that include optimal imaging strategies, the selection of the best thrombolytic agent, and the management of wake-up strokes? And in stroke systems of care, how do we determine who to transfer, when to transfer, and how to transfer patients with stroke in a timely manner, particularly in the era of severe hospital crowding, significant ED boarding, and critical health care workforce shortages (EMS, nursing, techs, and board-certified emergency physicians)?
Like other practices, we will need learning networks like E-QUAL and other systems of care with well-developed protocols including engaging our consultants to support treatment decisions. As we recognize the growing strength of our systems for acute stroke care, we have the tools and resources to provide optimal care for our patients. It is now imperative to push the conversations in our specialty to the next level, ensuring high quality care delivery and the best outcomes for our patients.
Pages: 1 2 3 | Single Page




No Responses to “Thrombolytics in Stroke: Moving Beyond Controversy to Comprehensive Care”