The Case
A 40-year-old man lost control while driving and collided into a barrier at 45 miles per hour. He was belted, no airbag was deployed, and there was no passenger intrusion. He did not lose consciousness and had full recollection of the event. He only complained of severe right knee pain.
Explore This Issue
ACEP Now: Vol 36 – No 05 – May 2017On examination, his primary survey was unremarkable. On secondary survey, there were no signs of head injury, but there was slight cervical spine tenderness without thoracic or lumbar spine tenderness. His chest and abdominal exams were normal. His focused assessment with sonography for trauma (FAST) exam was negative. His pelvis was stable. His extremity exam revealed a swollen tender right knee with an obvious effusion and very limited range of motion.
Discussion
One of the differential diagnoses that we don’t often think about is that of the occult knee injury. A cognitive forcing strategy should be employed every time we are confronted with a patient who presents to the emergency department with a significant knee injury but has a normal or near normal X-ray:
- Quadriceps tendon rupture
- Patella tendon rupture
- Lateral tibial plateau fracture
- Knee dislocation with spontaneous reduction
- Locked knee
- Compartment syndrome
Here, we will review some physical exam pearls to help improve our assessment of the knee and elucidate pitfalls in the diagnosis and management of one of the more serious but rare occult knee injuries. Spontaneously reduced occult knee dislocation is often missed and may result in ischemic complications culminating in limb amputation.
Knee Examinations in Patients with Severe Knee Pain
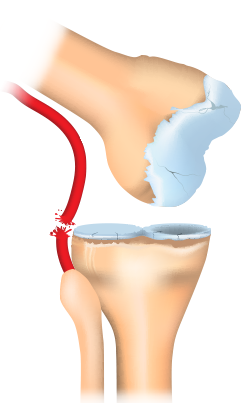
Posterior knee dislocation.
ILLUSTRATION: Chris Whissen & shutterstock.com
Many patients who have suffered an acute knee injury will experience pain that limits the physical exam. Clinicians may short-change their examination of the knee because they don’t want to cause more pain. Nonetheless, there are several tips to help patients relax enough to help facilitate provocative testing and the essential maneuvers. First, patients must be supine on a stretcher (not sitting in a chair), with both knees fully exposed. Place a pillow or roll under the distal femur so that the knee is relaxed at about 20 degrees of flexion to allow for provocative knee testing. If necessary, inject 3 mL of 1% lidoocaine into the knee joint before attempting provocative maneuvers.
The Case Continued
After placing a roll under the patient’s distal femur and injecting the knee joint with lidocaine, a full knee exam, including neurovascular examination of the lower extremity, was completed. This revealed normal pedal pulses bilaterally. However, there was significant ligamentous laxity of the knee. After the cervical spine was cleared and the patient was observed for six hours with serial examinations, he was placed in a full leg posterior splint and sent home with orthopedic follow-up.
Three days later, the patient returned to the emergency department with severe foot pain and a cold, pulseless foot. Emergency vascular surgery was performed for a massive popliteal thrombosis; he never recovered full function of his right lower extremity.
When to Suspect an Occult Knee Dislocation
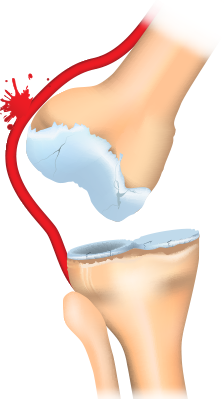
Anterior knee dislocation.
ILLUSTRATION: Chris Whissen & shutterstock.com
About 20 percent to 50 percent of all knee dislocations spontaneously reduce before patients arrive at the emergency department, and while patients may feel a shift of the knee joint, they may not recognize that their knee is dislocated. One pitfall in the history is assuming that a low-energy mechanism cannot cause a knee dislocation. A low-energy mechanism such as stepping off a curb in patients with a body mass index greater than 40 accounts for a significant proportion of missed occult knee dislocations. One study found that 47 percent of knee dislocations were due to low-energy trauma (eg, slips and falls), with 75 percent being in obese patients. Obese patients with low-energy trauma were more likely to have associated neurovascular injury than high-energy trauma patients in this cohort.
If patients have severe knee pain and a large effusion, check for a “loose knee.” Sometimes it is obvious that there is multidirectional ligamentous laxity when the examiner stabilizes the thigh and attempts to move the lower leg with the knee slightly flexed. A helpful rule of thumb is three of four knee ligament disruptions should be considered a knee dislocation until proven otherwise. Another clue: if patients complain of the knee buckling and are found to have a foot drop, then a knee dislocation should be suspected as the dislocation can cause a common peroneal nerve palsy. Lastly, upon lifting the patients’ legs by their heels, the dislocated knee may fall into hyperextension compared to the contralateral knee.
Workup of Suspected Knee Dislocation
The presence of normal distal pulses does not preclude occult popliteal artery injury as this has been shown to have a rate of 5 percent to 15 percent when normal pulses are present.
Ankle brachial index (ABI) and Doppler ultrasound imaging may miss small intimal injuries that clot after a few days. The gold standard is an arteriogram, but CT angiogram is more readily available.
Until recently, all patients with suspected knee dislocation underwent CT angiogram to assess for vascular injury. However, since the vast majority of patients who do have a vascular injury but have normal serial neurovascular exams and normal serial ABIs have intimal tears that do not require surgery, some experts recommend simply administering anticoagulants and admitting patients for observation without performing a CT angiogram.
If you suspect an occult knee dislocation, immediately consult orthopedics as revascularization within six to eight hours of popliteal artery injury is recommended to prevent ischemic complications.
Occult Knee Dislocation Take-Home
Don’t send home patients who tell you that it felt like their knee shifted out of place and they have a big swollen knee with laxity in multiple directions on exam until you’re sure they haven’t had a vascular injury related to a spontaneously reduced knee dislocation. Even if they have palpable peripheral pulses and a normal ABI, speak to your orthopedic surgeon, considering a CT angiogram to rule out a popliteal injury, and admit. Remember to have a high index of suspicion in any obese person with even a low-force mechanism.
A special thanks to Dr. Arun Sayal and Dr. Hossein Mehdian for their participation in the EM Cases podcast on which this article is based.
 Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Dr. Helman is an emergency physician at North York General Hospital in Toronto. He is an assistant professor at the University of Toronto, Division of Emergency Medicine, and the education innovation lead at the Schwartz/Reisman Emergency Medicine Institute. He is the founder and host of Emergency Medicine Cases podcast and website.
Pages: 1 2 3 | Multi-Page





No Responses to “Tips for Emergency Physicians on Spotting Occult Knee Dislocation”