Five years after the U.S. Department of Health and Human Services’ Office of the National Coordinator for Health Information Technology (ONC) developed the 21st Century Cures Act allowing patients expanded access to their electronic health records, the sweeping law is, for all practical purposes, in full effect. And although the increased transparency that the law represents is empowering to patients, it does require adjustments for physicians.
Explore This Issue
ACEP Now: Vol 41 – No 03 – March 2022“There’s always been this veil of mystery around physicians’ notes,” said Áine Yore, MD, an emergency physician affiliated with Providence Regional Medical Center in Everett, Washington. “Before [the Cures Act], if the patient wanted to see their whole chart, they would have to request it from a medical records department, pay a fee and maybe wait weeks for it to be released.” Today, patients log in to their record to easily view appointment information, medication lists, lab results and, now, physicians’ clinical notes.
Given this latest development, emergency physicians weigh in on the law’s unique impact in the emergency department.
Sparking a Conversation
Any patient who can connect to an online patient portal can gain access to their information, and this becomes a jumping-off point for doctor-patient discussion about their health status. “Patients accessing their information in real-time fuels more questions about their results, leading to meaningful conversations with physicians,” explained Indira Gowda, MD, an emergency physician at University of California Los Angeles Medical Center. “As a result, patients end up better informed.” The easy availability of information also enables patients to share it with family members or friends who may help them better interpret their results. “Research has shown this is especially true for non-English-speaking patients,” added Dr. Gowda.

Dr. Indira Gowda
To translate those real-time results into informative discussions, Dr. Yore is always prepared to give impromptu anatomy lessons in the patient room. “I’ll walk in and say, ‘You’ve got a kidney stone,’ and they’ll say, ‘Yeah, doctor, we know—we saw that an hour ago.’ And I’ll say, ‘Okay, well, very good, let’s talk a little more about this,’” she explained. “And that gives me an opportunity to provide more education.”
Another potential benefit can be seen in cases of incidental findings. “You do a chest X-ray to look for pneumonia, and it shows a spot on one of the lungs. Although this is a double-edged sword because now the patient sees this and the radiologist is saying, ‘Well, you have to rule out cancer,’ it also keeps us honest,” Dr. Yore said. “Maybe in the past some of us haven’t been too diligent about disclosing incidental findings and saying to patients, ‘This is probably nothing, but you do need to follow it up and get that CT in six months,’ or whatever the recommendation is. So the patient is now independently aware, and I think this increases our compliance to that communication with patients.”
The degree to which some of the benefits of the Cures Act apply to the emergency department setting is not clear. “[The Cures Act] is supposed to help improve the patient-doctor relationship and improve trust and communication amongst patients and providers, but this has only really been studied in nonemergency, acute care settings, such as the outpatient clinic,” said Dr. Gowda. One difference lies in the very nature of the emergency physician–patient relationship, which by nature is brief and limited, and any opportunity to educate patients plummets when that emergency department (ED) visit ends. Even patients who are inclined to reach out post-visit are likely to have a difficult time. “We come and we go. We work weird hours,” Dr. Yore said. “An oncologist’s relationship with their patient may be measured over months and years, whereas I have 180 minutes with each patient, by and large.”
Potential Pitfalls
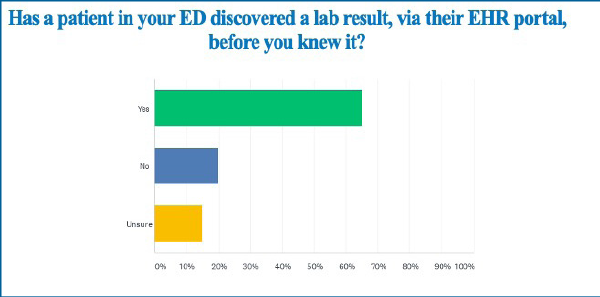
In a recent survey of ACEP members on the 21st Century Cures Act, two-thirds of 134 respondents reported cases where patients knew their test outcome before their clinician could discuss it with them. This increased the likelihood of patients discovering a bad result on their own. Dr. Gowda cites an instance in which a woman discovered that she had had a miscarriage by reading the final impression of her radiology report. “I feel like providing patients this information without a human interaction can create more harm than good,” she said.
A more common scenario is the patient who experiences undue anxiety over an abnormal but clinically irrelevant test result. “When an ED patient is scared and these results are trickling in electronically, a trivial abnormality or errant phrase may get magnified or misinterpreted,” explained Nicholas Genes, MD, PhD, FACEP, an emergency physician at New York University (NYU) Langone Health, clinical associate professor in the department of emergency medicine at NYU Grossman School of Medicine and chair of ACEP’s Health IT Committee. “I remember a patient with a history of anxiety who brought up so many details from prior notes that what should have been a quick visit ended up feeling like a cross-examination where I had to discuss my own and other doctors’ medical decision making. Being transparent is usually a great thing, but sometimes in a busy ER we don’t need to revisit clinical notes written months ago.”
Pages: 1 2 3 | Single Page





No Responses to “Tips for Adjusting to the New Cures Act Rules in Emergency Departments”