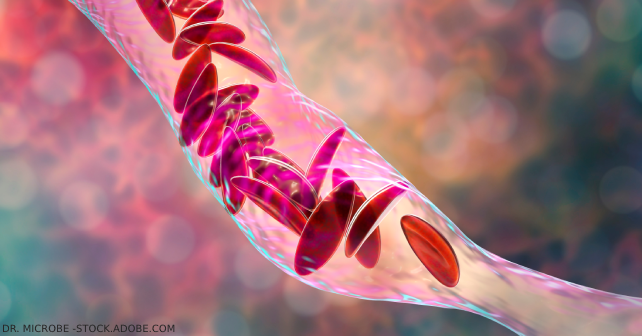
CVT is found most often in female patients 20 to 50 years of age.6 Risk factors include all the traditional thromboembolic risk factors including pregnancy, estrogen use, cancer, prolonged immobilization, etc., plus head and neck infections (leading to septic cavernous sinus thrombosis) and head trauma, including basal skull fracture.6
Explore This Issue
ACEP Now: Vol 42 – No 09 – September 2023Two key clinical features of advanced CVT are papilledema and loss of venous pulsations on fundoscopy.7 POCUS may aid in identifying papilledema by measuring optic nerve sheath diameter, however the accuracy of this finding depends on the skill of the clinician.8
To curb the urge to order a CT venogram on every patient with unexplained headache, D-dimer has been proposed as a screening test for patients with a low pretest probability of CVT. The sensitivity of D-dimer for the diagnosis of CVT ranges from 82 percent to 98 percent, which is not good enough to rule out the diagnosis with certainty but may shift one’s pre-test probability to aid in decision making around imaging.9,10 D-dimer should be reserved for low pretest probability patients and it should be recognized that utilization of D-dimer may increase CT venogram use.
Unenhanced CT may reveal a hyperdensity in the superior sagittal sinus (the “delta sign”) or straight sinus (the “dense cord sign”), but only in about 30 percent of cases. Hemorrhage, seen in about 30 percent of patients, is readily apparent on unenhanced CT. The findings of isolated bilateral frontal lobar or thalamic hemorrhages are another clue to the diagnosis of CVT on unenhanced CT.11
Once a diagnosis of CVT is made, it is imperative that these patients are started on either unfractionated or low-molecularweight heparin. A common pitfall is to withhold administration of heparin when CT reveals hemorrhage(s). Even though hemorrhage extension is found in 11 percent of patients with CVT, this does not seem to be related to anticoagulation.12 Intracranial hemorrhage is not a contraindication to heparin administration in patients with CVT.13
So when should we consider the diagnosis of CVT in patients presenting to the ED with headache? Otherwise unexplained headache in a young female with thromboembolic risk factors should prompt us to consider the diagnosis, perform a careful fundoscopic exam and consider a D-dimer in low-risk patients to help further risk-stratify patients. Patients with unexplained headache plus seizure, altered level of awareness, or focal neurologic sign(s) should also be considered for the diagnosis of CVT. Those patients with unremarkable unenhanced CT and LP findings, but with persistent unexplained headache and risk factors for CVT should, with shared decision making, be considered for a CT venogram done in the ED.
Pages: 1 2 3 | Single Page




No Responses to “Tips for Diagnosing Cerebral Venous Thrombosis in the Emergency Dept.”