Similarly, ultrasound (US) is of limited value for occult fracture confirmation. Certainly, US may be helpful with some soft tissue injuries. It is less helpful in fractures. The sensitivity and specificity of ultrasound in diagnosing radiographically occult scaphoid fracture ranged from 77.8 to 100 percent and from 71.4 to 100 percent, respectively, with pooled estimates of 85.6 percent (95% CI, 73.9–92.6%) and 83.3 percent (95% CI, 72.0–90.6%), respectively.5
Explore This Issue
ACEP Now: Vol 39 – No 03 – March 2020While there are suggestions in the literature that US may be an option for suspected scaphoid fractures, it is not considered sensitive enough to reliably alter ED management decisions.3,4
Case 2: Occult Lateral Tibial Plateau Fracture
A 78-year-old male presents with valgus stress to left knee, immediate pain, non-weight-bearing, and swelling within an hour. On exam, the knee is swollen, there is tenderness along the lateral joint line, the ligaments are stable, and soft tissues are intact. X-rays of the knee (four views) show effusion only.
Diagnosis: suspected occult lateral tibial plateau fracture.
Valgus stress with immediate pain, rapid swelling (implying acute hemarthrosis), and non-weight-bearing suggest a lateral tibial plateau fracture, especially in older patients with osteoporosis. On exam, the swollen knee, lateral joint line pain, and inability to bear weight are consistent with a likely tibial plateau injury. Even in the face of normal X-rays, the high clinical suspicion should make one pause and consider occult fracture. Such fractures are at risk of displacing if the diagnosis is missed in the emergency department and the patient is allowed to weight-bear.6
More tests? Or “treat and more time?” The option for treat and more time means immobilization, crutches, and non-weight-bearing. In many older patients, this proposition is very risky, so the push would be for advanced imaging (a CT scan) as soon as can be reasonably arranged. The patient should be kept non-weight-bearing until the diagnosis is clarified. A younger patient with a similar assessment may be more likely to manage crutches. Therefore, the option of immobilization, crutches, strict non-weight-bearing, and close follow-up (ideally within a week) may be more reasonable, depending on your local resources and preferences.
Case 3: Occult Hip Fracture
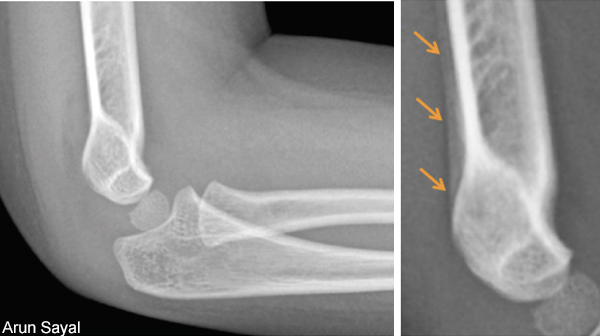
A 74-year-old female slips and falls. She has pain to the right hip and is non-weight-bearing. There is no limb-shortening or external rotation. She has a tender right hip and significant decreased range of motion (passive and active). X-rays of the hip and anteroposterior pelvis are normal.
Diagnosis: suspected occult hip (neck of femur) fracture.





No Responses to “Tips for Managing Suspected Occult Fractures”