The incidence of radiographically occult hip fracture (neck of the femur) is estimated to be between 5 and 10 percent—and more likely in elderly patients.
Explore This Issue
ACEP Now: Vol 39 – No 03 – March 2020A few important warnings about ED patients with hip fractures. The “classic” patient with a hip fracture has fallen and cannot walk, and their leg is short and externally rotated. Shortening and external rotation indicate a displaced fracture. However, an undisplaced hip fracture will not have the classic short and externally rotated presentation—it will have symmetric alignment to the contralateral leg. While most patients with a hip fracture are unable to walk, a minority of patients with an impacted, undisplaced hip fracture may be able to, albeit with a painful limp. In some cases, history (or lack thereof) can mislead us; hip fractures can occur without falling. In patients with an osteoporotic (weak), arthritic (stiff) hip, a vigorous twist can produce enough torque to cause a fracture. Not realizing this can be a diagnostic pitfall.
Often, an occult hip fracture needs surgical management. Delay in diagnosis increases morbidity as diagnostic delay is associated with greater displacement and more extensive surgery.3 Even mortality increases with delay to surgery.7 A 13 percent increase in the risk of mortality for every day of delay in surgery has been reported.8 Ideally, patients with a hip fracture should be operated on within 24 to 28 hours. However, the decision to operate cannot be made until the diagnosis is confirmed.
This case highlights that a greater imperative exists to diagnose these injuries, requiring more tests on the index visit. However, if the clinical setting is such that advanced imaging is not available, then bed rest and non-weight-bearing are mandated until a diagnosis is confirmed. Ideally, arrangements for advanced imaging should be made.
Two additional points: Older patients with osteoarthritis can have marginal osteophytes. On CT, these marginal osteophytes can simulate fractures in their periphery. Osteoporosis can also accentuate lucencies and nutrient vessels, again mimicking fractures and leading to false positive reads.
Analysis
In determining a management strategy (more tests versus more time), three main factors should be considered for patients with a suspected occult fracture:
- Diagnosis in question
- Patient in question
- Available resources
- Diagnostic Factors
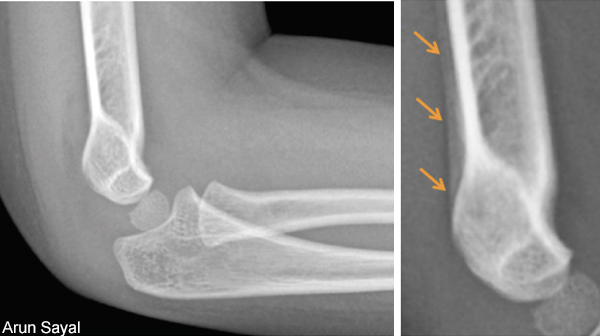
For some occult fractures, the plan of immediate immobilization and delaying diagnostic confirmation is reasonable since this strategy would not adversely affect outcome. However, diagnostic delay of other radiographically occult fractures can be harmful.9 Suspected scaphoid fractures with negative X-rays are the classic example. Suspected distal radius fractures can be approached similarly. Most pediatric cases of suspected occult fractures can be managed this way.





No Responses to “Tips for Managing Suspected Occult Fractures”