
Explore This Issue
ACEP Now: Vol 40 – No 06 – June 2021Figure 2A: For a distal sciatic nerve block in the popliteal fossa, the clinician has stabilized their nondominant hand during the block.
Figure 2B: Once the needle has entered the soft tissue, gentle probe manipulation (fananing or rotating) can allow for proper needle visualization.
After skin puncture, alternating subtle transducer movements with gentle needle manipulation will allow the needle tip to come into view. If the needle is not already in view, close attention to tissue deformation with needle movement will give clues as to its location. If needle sight is lost, take a moment to look away from the display screen to visually inspect the transducer position on the skin and its relationship to the needle’s path. The transducer can then be fanned or rotated to visualize the needle clearly (see Figure 2B).1
Optimizing Needle Visualization by “Toeing In” the Transducer
Needle visualization during in-plane ultrasound-guided nerve blocks with a steep needle trajectory is particularly challenging. Adjusting the “angle of insonation” can produce a crisp, clear image of the needle as it travels toward its intended target.
The angle of insonation refers to the angle at which an ultrasound beam intersects the nerve block needle. The smooth, metallic surface of the needle effectively functions as a mirror for ultrasound waves, thus small changes to the angle of the needle greatly influence its visualization (see Figure 3).2 If the ultrasound beam is perpendicular to the needle (ie, angle of insonation of 90 degrees), the majority of ultrasound waves are reflected back toward the transducer, creating a bright, clear image of the needle (see Figures 3B and 4B).3 Unfortunately, deeper targets necessitate a steeper needle trajectory and therefore create a lower angle of insonation. The result is that the majority of ultrasound waves are reflected away from the transducer and the needle is poorly visualized (see Figures 3A and 4A).
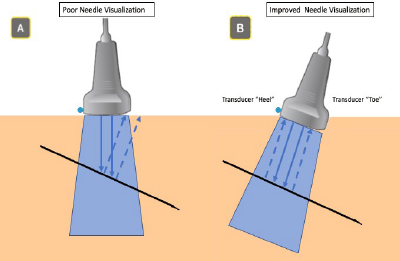
Figure 3A: Low angle of insonation: some ultrasound waves are reflected away from the transducer.
Figure 3B: High angle of insonation: a majority of ultrasound waves are reflected toward the transducer.
To effectively raise the angle of insonation (and thereby optimize needle visualization), an operator may rock or “toe in” the ultrasound transducer (see Figure 5).3 This is best achieved by pressing one end (the “toe”) of the transducer deeper into the superficial soft tissue so that the trajectory of the transducer more closely mimics the trajectory of the needle (see Figure 5B). A generous allocation of ultrasound gel can help ensure the other end of the transducer (the “heel”) maintains contact with the skin surface. For very deep targets, switching from a linear to a curvilinear transducer will facilitate more exaggerated toeing/rocking and improved deep structure resolution. Also, many commercial nerve block needles have etched patterns which serve to make the needle tip more echogenic. Use of such needles can further enhance needle visualization, particularly for nerve blocks necessitating a steep angle of approach.2,3
Pages: 1 2 3 4 | Single Page




No Responses to “Tips for Performing Ultrasound-Guided Nerve Blocks in the Emergency Department”