The Case
A 28-year-old male presents after a motorcycle crash. He has right lower leg pain and tenderness. His pulses and nerve function are intact. An X-ray shows a tibial shaft fracture. After splinting the leg and calling orthopedics, the physician finds the patient is anxious and reporting worsening pain despite IV morphine. His leg has become pale and cool, with absent pulses.
Explore This Issue
ACEP Now: Vol 38 – No 10 – October 2019Clinical Presentation
This textbook presentation of compartment syndrome seems easy. Real cases often are not. In emergency medicine, we deal with critically ill patients who may require sedation and/or intubation, and diagnosing compartment syndrome in patients can require some finesse. Not only can compartment syndrome cause major complications, but frighteningly, 23 percent of medicolegal cases involving compartment syndrome were due to misdiagnosis, while 32 percent of cases were due to delayed treatment.1
Compartment syndrome is due to excessive pressure in a fascial compartment, either through increased volume in a fixed compartment (edema, hematoma) or reduced size of a compartment (tight cast, wound dressings, poor body positioning, etc.).2-4 As pressure builds, lymphatic, capillary, and venous blood flow decrease.5-7 This results in reduced arterial blood flow and tissue ischemia, followed by necrosis, neurological damage, contractures, and, in severe circumstances, need for amputation.8-11 Rhabdomyolysis may also occur with muscle breakdown.8-11 Unfortunately, muscle necrosis can occur quickly; in one study, one-third of cases experienced muscle necrosis within three hours of injury.12
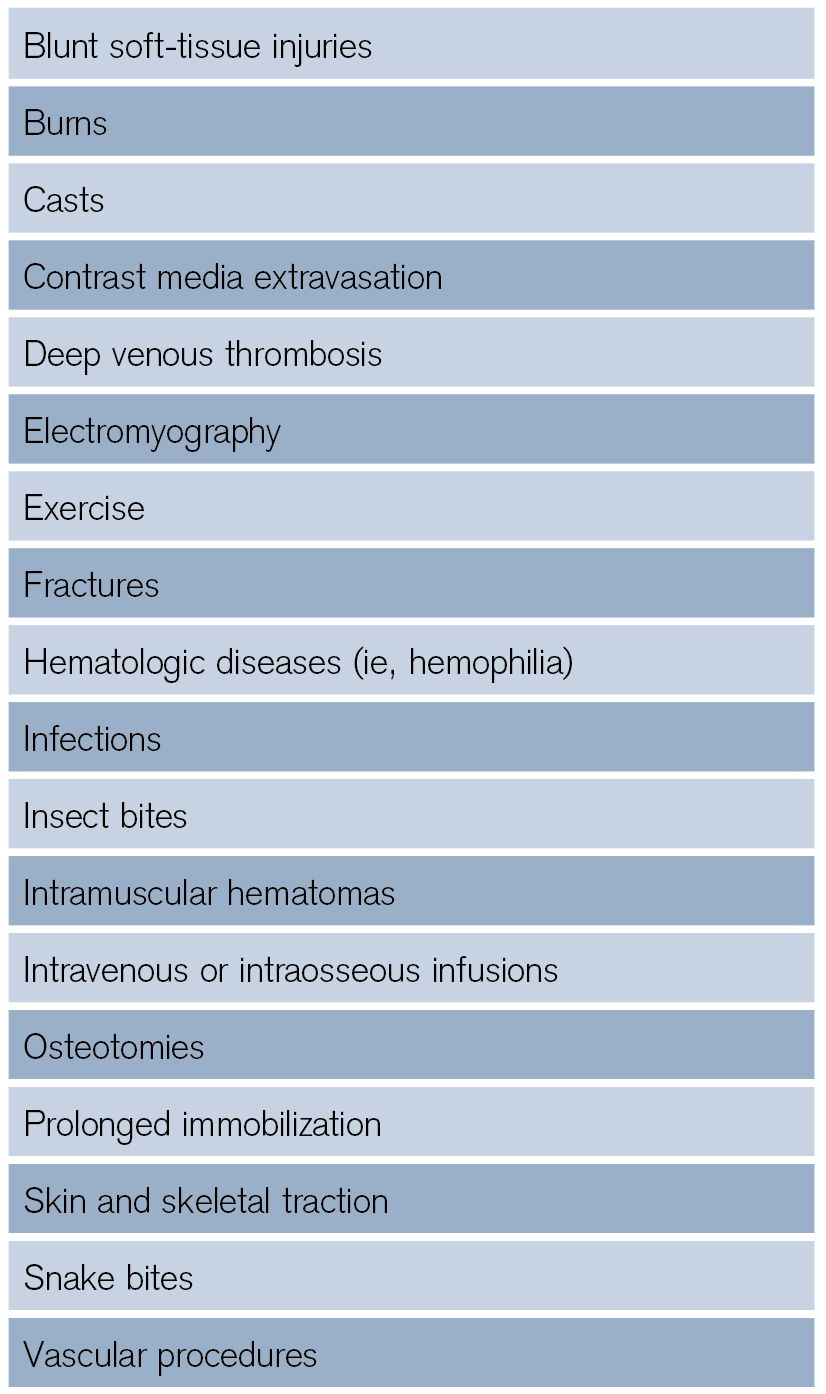
The most commonly affected region is the anterior compartment of the lower leg, and compartment syndrome can occur in up to 10 percent of patients with tibial fracture.5,6,13-15 Male patients age 20 to 40 years are particularly at risk, as this age group has a higher risk of high-energy injuries, greater muscle bulk (more swelling), and stronger fascia. However, the elderly are also at higher risk due to baseline hypertension and reduced compartment perfusion.4 Fractures are the most common etiology. Open fractures can also cause compartment syndrome, as the small fascial/skin breaks do not adequately release pressure.13,16-18 Other causes are shown in Table 1.
How useful are historical features? Unfortunately, early findings can be subtle or not detected in patients with altered mental status, major trauma, substance use, and extremes of age.2-4,18 Classically, the earliest symptom is pain out of proportion to the exam (as with other conditions including necrotizing fasciitis and mesenteric ischemia). Patients typically describe this pain as a deep, severe pain that worsens with passive stretch.3,19-21 While this seems relatively straightforward, data suggest that severe pain has poor sensitivity, as pain is typically subjective.19 If ischemia develops, pain may vanish with necrosis.18 Other late symptoms include sensory changes/paresthesias and focal motor deficits.5,6,19
Pages: 1 2 3 4 | Single Page





3 Responses to “Tips for Quickly Diagnosing Compartment Syndrome”
November 19, 2019
Emil Pajek MDCannot find the CME that is listed in the article.
ALSO the article in the magazine has DIFFERENT Title than here …cannot find the CME /article or reference.
I had to call the ACEP
February 4, 2020
David GlassSame. I can’t find the CME link / test.
March 20, 2021
J WellsI think you mean AP is diastolic pressure minus compartment pressure