SE is defined as seizure activity lasting more than five minutes or recurrent seizures without recovery in between.11,13 It is the most common neurological emergency in childhood.13 Prolonged seizure activity can permanently damage neurons; the longer a seizure lasts, the less likely it is to stop spontaneously and the less likely it is to respond to standard antiepileptic drugs (AEDs).3 SE appears to increase expression of drug efflux proteins in the brain, thus decreasing AED levels there.13 As it is impossible to predict how long a given seizure will last, it’s best to administer appropriate medications without delay by the fastest reliable route available and escalate therapy as necessary. Intramuscular midazolam administration has been shown to be safe and effective for prehospital SE.12 IV access can be challenging in seizing children, especially if the veins were extensively used in the past. An intraosseous line can be lifesaving in this situation. Early cardiorespiratory monitoring and supplemental oxygen are recommended for all patients.
Explore This Issue
ACEP Now: Vol 37 – No 11 – November 2018For suggested diagnostic workup of SE, see Table 2. For medication sequence in treating SE, refer to Table 3. Both seizure activity and medications used to terminate it can cause respiratory failure. Bag-valve-mask ventilation can sometimes stave off the need for endotracheal intubation unless emergent imaging or other diagnostic procedures are immediately needed. In case of ongoing seizure activity or altered mental status, EEG monitoring is recommended early.11,13
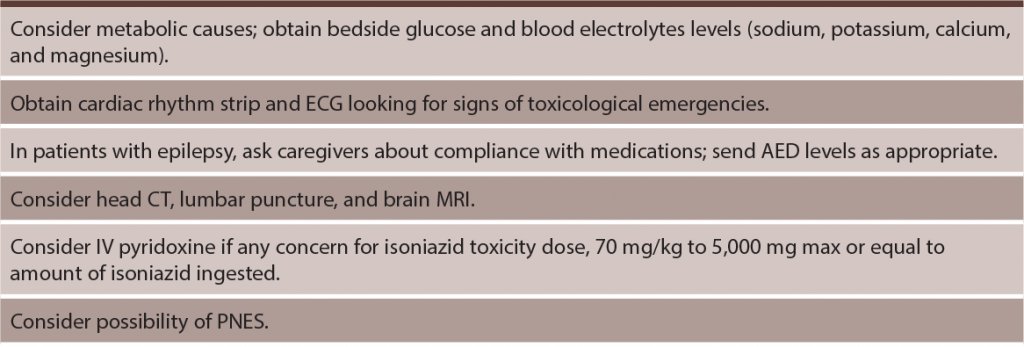
(click for larger image) Table 2: Important Diagnostic Tests for Patients in Status Epilepticus11,13
Nonconvulsive SE (NCSE)
Prolonged brain seizure activity on EEG in a patient with altered mental status but without convulsions defines NCSE. It can present separately as an acute confusional state or develop following an observed seizure.11 A wide variety of symptoms have been described, ranging from aphasia to severe agitation or coma.11 It appears to have a similar incidence in children and adults and is not rare.14,15 In settings where immediate EEG is not available, its recognition can be quite challenging. In our experience, in unclear cases, cautious administration of a weight-appropriate benzodiazepine dose can, at times, result in dramatic improvement in mental status aiding in diagnosis. Similarly to patients with convulsive SE, these patients need emergent workup focusing on diagnosing life-threatening etiologies, continuous EEG monitoring, and expeditious AED administration. As is the case with convulsive SE, the prognosis mostly depends on etiology and the degree of neurological impairment.13
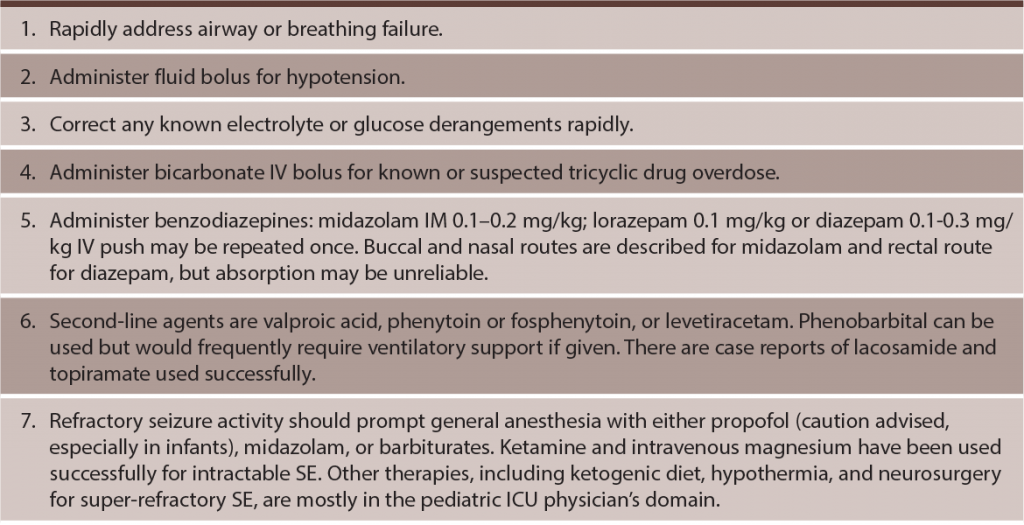
(click for larger image) Table 3: Suggested Intervention Sequence in Treatment of Pediatric Status Epilepticus3,11–14,18,19
Psychogenic Nonepileptic Seizure (PNES) and Other Seizure Mimics
PNES is defined as repeated and frequently intractable seizure activity in the absence of epileptogenic changes on concurrently recorded EEG.16 Video EEG is necessary to firmly establish the diagnosis, and psychiatric comorbidities are common in both PNES and epilepsy.16 As many as a quarter of children thought to be suffering from seizures are ultimately found to have PNES.17 Misdiagnosis leads to inappropriate use of antiepileptic drugs with corresponding side effects up to and including the need for mechanical ventilation. Appropriate referral and treatment achieved an 80 percent remission rate in one study.17
Special Populations

(click for larger image) Table 4: Select Antiepileptic Drugs (AEDs)2,3,8,20
While numerous new AEDs are now available, it’s unknown if they are any more effective and safer than the old ones.21 While AEDs can lower the chance of a seizure occurrence, they do not treat epilepsy or prevent the development of it.
NOTE: AEDs with US Food and Drug Administration boxed warnings are carbamazepine, felbamate, lamotrigine, perampanel, and valproic acid
Pages: 1 2 3 4 5 | Single Page





No Responses to “Tips for Updating Your Approach to Pediatric Seizures”