
Explore This Issue
ACEP Now: Vol 37 – No 04 – April 2018Figure 3: Think of the airway in these three sections.
PHOTO: Richard Levitan
Supine positioning runs counter to lower airway (alveolar) patency. In the supine position, the lung’s upper areas compress the dependent alveoli, and abdominal contents push the diaphragm up, significantly reducing lung volume. Changing position from upright to supine reduces functional residual capacity (FRC) by as much as one liter. Because estimated FRC in adults measures approximately 2,400 ml, a reduction of 1,000 ml reduces FRC by 42 percent. Loss of tone (as occurs with anesthetic induction) or over-sedation further reduces FRC by 400 ml.
Collectively, then, FRC reduction from standing to supine plus loss of tone results in a reduction of roughly 52 percent! This reduction’s impact on alveolar gas absorption is dramatic, especially in patients who already have compromised lung function.
Sit Them Up
The first and most important technique for boosting oxygen absorption is to apply high oxygen concentration with high flow as a means of augmenting the patient’s negative inspiratory efforts. But beyond the application of 100 percent oxygen, and shy of extracorporeal membrane oxygenation or using hyperbaric oxygenation, clinicians have only two methods of further improving oxygenation across the alveoli: 1) positioning, and 2), positive end-expiratory pressure (PEEP).
The immediate and easiest positioning fix to open the lower airway? Sit the patient up. This causes the abdominal contents to move caudad, the diaphragm to drop, and lung volume to rapidly expand. The area for gas absorption across the alveioli dramatically increases with proper positioning.
Middle airway obstruction is an infrequent clinical problem because the three-dimensional shape of laryngeal cartilages and the cartilaginous rings of the trachea maintain patency regardless of positioning or muscular tone. An orally placed tracheal tube traverses the upper airway and reaches the mid-trachea level. When the middle airway obstructs due to intrinsic laryngeal-tracheal pathology (eg, tumors, angioedema about the larynx, blood clots, etc.) or trauma (eg, laryngeal fracture, direct tracheal injury, etc.), patients can die precipitously.
With an awareness of gravity and positioning, and an understanding of the three airway components, engineering airway interventions that augment patency and gas absorption makes sense. Here’s my stepwise approach to hypoxia with procedural sedation or in an initial emergency department presentation:
- Sit the patient up, allowing the diaphragm to drop and the alveoli volume to expand, and pull on the mandible. This opens the upper airway.
- Send O’s up the nose—blast open the soft palate and shoot oxygen into the trachea up to and beyond 15 lpm.
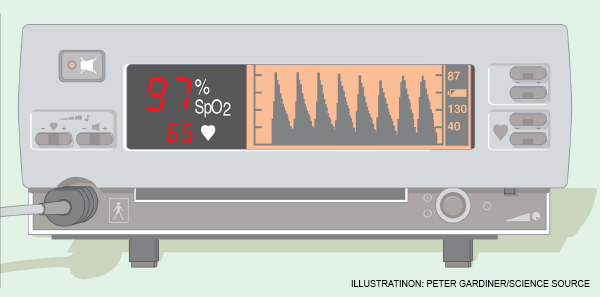
- Add PEEP with a bag valve mask (BVM) and a PEEP valve, or a continuous positive airway pressure system. PEEP is absolutely necessary when high-flow oxygen (with cannula plus mask) does not achieve high oxygen saturations (ie, >98 percent).
To desaturate after the tracheal tube has been placed, first examine the system to ensure the tube is at right depth, the oxygen is connected, and the cuff is up. Suction through the tube to remove mucous plugs, clots, etc. If high-pressure alarms go off or bagging difficulty persists (that is not consistent with the patient’s pathology, ie, COPD, asthma, etc.), pull the tracheal tube. It is quite common to experience ball-valve obstructions from mucous plugs or clots that suctioning alone doesn’t resolve.
Pages: 1 2 3 | Single Page






No Responses to “Tips to Improve Airway Management”