
The insurance industry poses a very significant challenge that necessitates constant vigilance of critical indices of EM practices, resulting in a new “EM Triple Aim.” The announcement by Aetna, Humana, and UnitedHealthcare of the publication of reimbursement data represents a watershed moment in payer-provider relations. This is a calculated move requiring constant monitoring and may very well be followed by similar moves by other payers. Why the monitoring vigilance? It is important to remember that over the past 20 years virtually every payer has gone through a class-action settlement for inappropriate denials and/or payments to physician practices. The result of these settlements has been the payout to physicians of millions of dollars. These payments came, of course, years after the services were provided. Now, we fast-forward to today, with three major payers mirroring the Medicare announcement. EM physicians, take note—these maneuvers change the contracting landscape significantly. The new “EM Triple Aim” will be:
Explore This Issue
ACEP Now: Vol 33 – No 09 – September 2014Acuity mix of the EM practices monitoring.
Baseline/benchmark contractual payment tracking and monitoring.
Claims denials monitoring and resultant appeal processing.
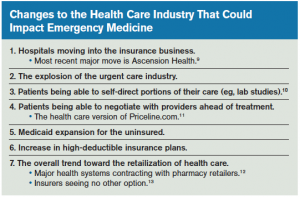
The necessity of monitoring practice acuities is warranted by the macro industry shifts noted above. The urgent care boom will certainly drain some of the lower acuity mix patients from the ED. However, until the primary care network is capable of handling the newly insured, the ED remains the option of choice for these patients. As the former change (the urgent care boom) erodes the lower ED acuities, the overall practice acuities stand to increase. The combination of these patient acuity changes and the coincidental demographic changes absolutely mandates these practice indices be watched constantly because they can have significant impacts on the financial standing of EM practices.
Baseline/benchmark contractual payments likewise require vigilance to first ensure the accuracy of the payments. It will additionally be prudent to fortify and substantiate the quality and value metrics indigenous to every EM practice when engaging any payer in a contract negotiation or renegotiation. The payer-industry tactic of mirroring moves by Medicare needs to be recognized as a forerunner for payers to potentially try “negotiating rates down” for EM practices. It is incumbent on every EM practice to be prepared for this possibility and to be ready with both a strong data and quality/value position when engaging payers. EM simply cannot survive as we know it at Medicare reimbursement rates. It is imperative we be fully armed with strong data metrics coupled with a quality/value proposition when engaging payers.
Pages: 1 2 3 4 | Single Page



No Responses to “Top Concerns for Emergency Medicine Today”