
Explore This Issue
ACEP Now: Vol 33 – No 09 – September 2014Donald Berwick, MD, first coined the term “Triple Aim” for the goals of the emerging health care world.1 Emergency medicine has clinical ABCs as cornerstones of the specialty. Today, as the new health care world emerges, there are significant challenges and opportunities that will redefine the meaning of EM’s practice management ABCs; a new “EM Triple Aim” is at hand.
The first significant impetus to change was the Centers for Medicare & Medicaid Services (CMS) announcement making provider payment data available to the public.2 This change now provides critical information to everyone on how physicians have been paid by Medicare. In the context of other changes, this initial move by CMS will likely stand as an industry cornerstone/landmark change as it will have an impact throughout the provider community.
The second industry move of importance for physicians was the recent announcement by Aetna, Humana, and UnitedHealthcare of virtually the same change, namely the release of their payment data to the public.3
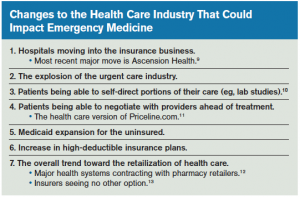
Along these same lines, it is important to recognize a very important article by Bob Herman, in which he potentially links the first two and begins exploring the potential for Medicare to become the health care industry’s sole payer.4 Although the article itself addresses hospital finances, it is prudent to take note of it. This may not be as far-fetched as one might think. Emergency physicians need to be armed with the facts and prepared to aggressively deal with several related changes and industry maneuverings that could potentially have a dramatic impact on the finances and even the survival of individual EM practices (see sidebar).
What might these changes mean for EM? These are major structural changes and shifts in the macroeconomic and demographic landscape that could have significant impact EM practices. The big-picture issues involve hospitals maneuvering to engage the insurance industry. Medicaid expansion certainly offers the potential for EM reimbursement to increase at least slightly, but it will be dependent on the actual levels of reimbursement. The explosion of the urgent care industry coupled with the retailization of health care definitely have the potential to significantly change the acuity mix of EM practices.
The insurance industry poses a challenge that necessitates constant vigilance of critical indices of EM practices.
Simultaneous, with these changes, we are living in an emerging health care world of physician engagement, alignment, and integration, with the hospital C-suite expecting the physician community to “get on board” with these changes that are beginning to significantly impact hospital finances. A hallmark of EM is its central role in triggering hospital admissions, with the emergency department accounting for at least 68 percent of hospital admissions.5 This landscape is, however, changing as hospitals move toward providing more care in outpatient settings. As the latter occurs, it can have a devastating financial impact on hospital finances, especially if hospital admissions substantially decline, which has been seen recently in suburban Philadelphia.6 The central role of EM in the hospital admission issue remains paramount.
The insurance industry poses a very significant challenge that necessitates constant vigilance of critical indices of EM practices, resulting in a new “EM Triple Aim.” The announcement by Aetna, Humana, and UnitedHealthcare of the publication of reimbursement data represents a watershed moment in payer-provider relations. This is a calculated move requiring constant monitoring and may very well be followed by similar moves by other payers. Why the monitoring vigilance? It is important to remember that over the past 20 years virtually every payer has gone through a class-action settlement for inappropriate denials and/or payments to physician practices. The result of these settlements has been the payout to physicians of millions of dollars. These payments came, of course, years after the services were provided. Now, we fast-forward to today, with three major payers mirroring the Medicare announcement. EM physicians, take note—these maneuvers change the contracting landscape significantly. The new “EM Triple Aim” will be:
Acuity mix of the EM practices monitoring.
Baseline/benchmark contractual payment tracking and monitoring.
Claims denials monitoring and resultant appeal processing.
The necessity of monitoring practice acuities is warranted by the macro industry shifts noted above. The urgent care boom will certainly drain some of the lower acuity mix patients from the ED. However, until the primary care network is capable of handling the newly insured, the ED remains the option of choice for these patients. As the former change (the urgent care boom) erodes the lower ED acuities, the overall practice acuities stand to increase. The combination of these patient acuity changes and the coincidental demographic changes absolutely mandates these practice indices be watched constantly because they can have significant impacts on the financial standing of EM practices.
Baseline/benchmark contractual payments likewise require vigilance to first ensure the accuracy of the payments. It will additionally be prudent to fortify and substantiate the quality and value metrics indigenous to every EM practice when engaging any payer in a contract negotiation or renegotiation. The payer-industry tactic of mirroring moves by Medicare needs to be recognized as a forerunner for payers to potentially try “negotiating rates down” for EM practices. It is incumbent on every EM practice to be prepared for this possibility and to be ready with both a strong data and quality/value position when engaging payers. EM simply cannot survive as we know it at Medicare reimbursement rates. It is imperative we be fully armed with strong data metrics coupled with a quality/value proposition when engaging payers.
Regarding payments, there is a new special case today for EM. The ever-increasing incidence of the new self-pay patient, engendered by the increasing incidence of high-deductible insurance patients, requires new patient follow-up techniques and protocols. As a first step, the quality of patient ED registration data and information becomes critical. The self-pay patient has always been a nemesis for EM practices, and we now have a new category of these patients. This impacts cash flow and the overall financial strength of EM practices. Payments by these patients need constant monitoring and new and creative follow-up protocols.
The issue of claims denials and appeals is important even along with a move toward partnering with payers, which in some instances can be part of hospital plans regarding physician integration. It is one thing to consider closer relationships with payers, but it is also imperative to be fully knowledgeable of the insurance industry’s historical track record, both before and after the numerous class-action settlements. The Medicare program today, its payments and denials, necessitates strong management and monitoring as evidenced in the recent lawsuit filed by several hospitals against the Department of Health and Human Services, with millions of dollars remaining outstanding due to substantial appeal backlogs.7 Today’s denials processing for hospitals and physician groups requires aggressive revenue-cycle tracking and follow-up protocols coupled with technological tools that can wrap and send all appeals and required supporting documentation quickly and expeditiously to payers. The market is changing on a daily basis, and it is imperative for EM practices to rethink, retool, and aggressively monitor these practice indices along with all other standard indices to ensure the financial health and strength of the specialty. The most recent alarm is sounded by Medscape Medical News journalist Robert Lowes, who notes that the Affordable Care Act rollout involving exchanges is causing significant accounts-receivable issues, which is again a warning for EM practices.8
EM has its own “Triple Aim” and a new practice-management ABC protocol. Acuities, baseline/benchmark payments, and appeals/denials analysis require strong management, constant monitoring, and sophisticated tools to ensure the financial strength and longevity of EM practices. As the landscape continues to substantially change, EM practices must adjust to meet these challenges. It is an opportunity to emerge as strong financial leaders in this new world.
 Mr. Holstein is director of business development for Zotec Partners in Bala Cynwyd, Pennsylvania.
Mr. Holstein is director of business development for Zotec Partners in Bala Cynwyd, Pennsylvania.
References
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health and cost. Health Aff (Millwood). 2008;27:759-69.
- Centers for Medicare & Medicaid Services. Medicare Provider Utilization and Payment Data. Centers for Medicare & Medicaid Services Web site. Available at: http://www.cms.gov. Accessed April 9, 2014.
- Demko P. Health insurance giants to make payment data accessible to public. Modern Healthcare Web site. Available at: http://www.modernhealthcare.com/article/20140514/NEWS/305149981. Accessed August 1, 2014.
- Herman R. What if Medicare were the only payer? Becker’s Hospital Review Web site. Available at: http://www.beckershospitalreview.com/finance/what-if-medicare-were-the-only-payer.html. Accessed August 1, 2014.
- Augustine J. Survey: the ED is the nexus of care. Emergency Physicians Monthly Web site. Available at: http://www.epmonthly.com/features/current-features/survey-the-ed-is-the-nexus-of-care/. Accessed August 1, 2014.
- Herman B. Crozer-Keystone Health System facing steep losses, low admissions. Becker’s Hospital Review Web site. Available at: http://www.beckershospitalreview.com/finance/crozer-keystone-health-system-facing-steep-losses-low-admissions.html. Accessed August 1, 2014.
- Adamopoulos H. Hospitals sue HHS over Medicare appeals. Becker’s Hospital Review Web site. Available at: http://www.beckershospitalreview.com/finance/hospitals-sue-hhs-over-medicare-appeals.html. Accessed August 1, 2014.
- Lowes R. Most medical groups are in ACA exchanges and dislike it. Medscape Medical News Web site. Available at: http://www.medscape.com/viewarticle/825732. Accessed August 1, 2014.
- Evans M. Ascension considers major insurance play. Modern Healthcare Web site. Available at: http://www.modernhealthcare.com/article/20140522/NEWS/305229947. Accessed August 1, 2014.
- Snow B. Online blood work: no doctor’s visit required. Fox News Web site. Available at: http://www.foxnews.com/health/2014/04/05/online-blood-work-no-doctors-visit-required. Accessed August 1, 2014.
- Dunn L. Priceline.com for healthcare? Yes, please. Becker’s Hospital Review Web site. Available at: http://www.beckershospitalreview.com/healthcare-blog/priceline-com-for-healthcare-yes-please.html. Accessed August 1, 2014.
- Robeznieks A. CHE Trinity, Walgreen enter coordinated-care agreement. Modern Healthcare Web site. Available at: http://www.modernhealthcare.com/article/20140521/NEWS/305219963. Accessed August 1, 2014.
- Williams KB. Why insurers have no choice but to hire retail execs. Healthcare Dive Web site. Available at: http://www.healthcaredive.com/news/why-insurers-have-no-choice-but-to-hire-retail-execs/265614. Accessed August 1, 2014.
Pages: 1 2 3 4 | Multi-Page



No Responses to “Top Concerns for Emergency Medicine Today”