Sciatica is radicular pain radiating down the buttocks along the course of the sciatic nerve. It is a common cause of low back pain, a complaint responsible for up to 2.7 million or 2.4 percent of annual United States emergency department (ED) visits.1, 2
Explore This Issue
ACEP Now: Vol 41 – No 06 – June 2022Typically, the ED treatment of sciatica pain is limited to various analgesic regimens. Nonsteroidal anti-inflammatory drugs (NSAIDs) provide superior pain relief when compared to placebo.3 Opioids are commonly used in the treatment for sciatica, however, the long-term potential for misuse and abuse drastically decreases their utility outside of the ED.4 In addition, recent data demonstrate that a single dose of opioids in the ED is not superior to alternatives.5 With such limited options for managing acute pain, additional modalities are needed.
The ultrasound-guided transgluteal sciatic nerve block (TGSNB)—a relatively new block—was first described in 2019 in emergency medicine literature as an analgesic technique for radicular sciatic pain.6 The TGSNB targets the sciatic nerve in the proximal leg leading to radicular pain relief. Although commonly used in anesthesia literature for orthopedic and podiatry surgeries, TGSNB utilization was uncommon until a recent case series demonstrated its superior pain relief in acute sciatica.6 Given the high volume of patients with sciatica in the ED, the TGSNB offers a highly effective or adjunctive pain treatment modality for many ED patients.
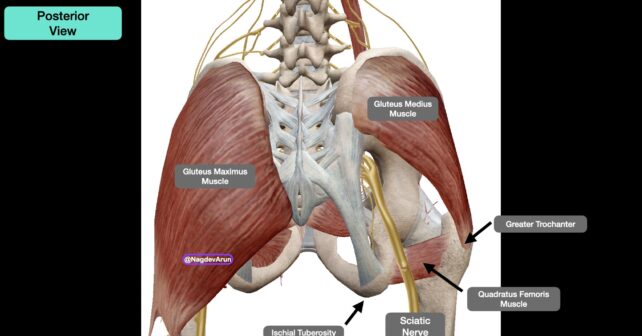
PICTURE 1 (click to enlarge): Anatomy image from the posterior view with relevant anatomy. On the right side, the gluteus maximus is left intact. On the right, the gluteus maximus has been removed so that the sciatic nerve can be clearly visualized running above the quadratus femoris muscle, and between the great trochanter (lateral) and ischial tuberosity (medial).
Anatomy and Innervation
The TGSNB targets the sciatic nerve at the level of the greater trochanter. Anatomically, the sciatic nerve is identified inferior to the gluteus maximus muscle as it courses adjacent to the ischial tuberosity (medially) and greater trochanter (laterally) (Picture 1). The sciatic nerve provides sensory innervation to the skin of the lower foot and lower leg. The medial aspect of the lower leg is innervated by the saphenous nerve. The peroneal branch of the sciatic nerve provides motor innervation to the muscles that dorsiflex the foot. As we are providing anesthetic proximally, one potential temporary side effect of the TGSNB is a foot drop.
Supplies
- Low-frequency curvilinear transducer (5–1 MHz) allows for greater visualization of the sciatic nerve and surrounding landmarks given their depth. In thin patients, and when learning to locate relevant anatomy, a high frequency linear transducer may be used (13–6 MHz).
- Anesthetic: 10 ml of 0.5 percent bupivacaine (5 mg/mL; maximum 2 mg/kg). Optional: 4–8 mg of dexamethasone may be added to increase half life of the bupivacaine.
- One 10 cc normal saline flush to hydro-dissect the sciatic nerve away from the gluteus maximus.
- 100 mm 21 gauge blunt-tip block needle or 20–22 gauge Quinke spinal needle (90 mm). Needle visualization for deep target blocks is significantly easier when using echogenic block needles.
- 91 cm or 36 inch tubing (if not using a block needle).
- Chlorhexidine skin prep.
- Transparent dressing (Tegaderm) for the transducer and sterile gel-packets.
- 25–30 g needle for local skin wheal.
Procedure
1. Pre-block
The clinician should be knowledgeable of the signs, symptoms, and treatment of local anesthetic systemic toxicity (LAST) and have 20 percent lipid emulsion therapy readily available for this rare but potentially serious complication. We recommend placing the patient on a monitor.
Pages: 1 2 3 4 | Single Page





No Responses to “How To Relieve Sciatica Pain with New TransGluteal Nerve Block Treatment”