Approximately 60,000 to 100,000 patients die from pulmonary embolism (PE) each year in the United States, and PE is the third leading cause of cardiovascular mortality.1
Explore This Issue
ACEP Now: Vol 43 – No 12 – December 2024A wide spectrum of severity exists in PE presentations, ranging from mild shortness of breath to cardiac arrest. A PE is classified into one of three categories: low risk, submassive, and massive. Low-risk and submassive PEs do not have hemodynamic compromise (i.e., no hypotension). A submassive PE does not result in hypotension but does result in right ventricular (RV) dysfunction (as evidenced by CT or ECG) and/or signs of myocardial injury, such as elevated B-type natriuretic peptide, elevated troponin, or new ECG changes. A massive PE, the most severe, causes hemodynamic instability and carries the most morbidity and mortality.2 With varying clinical pictures, unique patient profiles, and risk factors, the treatment of PE provides complex challenges.
Thrombolysis
Although systemic thrombolysis has been the standard treatment for submassive and massive PEs, its risk of major bleeding and intracranial hemorrhage continues to raise concern, particularly in older patients with comorbidities.3 Use of systemic thrombolysis carries a 20 percent risk for major bleeding, including a two to three percent risk for intracranial bleeding.3 Therefore, new interventions using catheter-based or mechanical removal strategies are becoming increasingly more common for the treatment of PE causing hemodynamic instability, myocardial injury, or severe hypoxia.3,4 In addition, for patients with contraindications or those who have failed thrombolysis, catheter-directed thrombolysis and surgical thrombectomy are useful treatment modalities that are associated with low major complication rates and improved patient outcomes.5
As opposed to systemic therapy, catheter-directed thrombolysis is a minimally invasive technique that delivers targeted lytic therapy locally to the clot using catheterization. Ekosonic Endovascular System (EKOS), a form of pharmacomechanical thrombolysis, uses a catheter to deliver thrombolytics directly to the target pulmonary artery in combination with high-frequency ultrasound to enhance lytic penetration and encourage thrombus fragmentation.6,7 Moreover, as the risk for bleeding with systemic thrombolytic therapy is dose-dependent, catheter-directed thrombolysis (CDT) allows for use of lower doses, making its use appropriate even for patients with relative contraindications.8 The prospective SEATTLE II trial demonstrated that this unique approach to thrombolysis therapy reduced clot burden, improved RV function, and reduced pulmonary hypertension, all while minimizing occurrence of intracranial hemorrhage in patients with massive and submassive PE.6
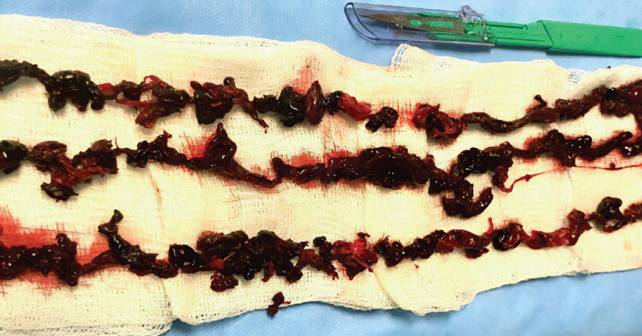
The second common catheter-directed approach is mechanical thrombectomy. This approach may be used as monotherapy or in combination with lytic therapy based on the clinical picture. The Inari FlowTriever System treats PE without the use of thrombolytics by using a large lumen catheter and large-bore syringe to mechanically remove large volumes of clots via aspiration.4,9 The FLARE study, a prospective multicenter trial, demonstrated that implementation of Inari FlowTriever in management of PE provided rapid thrombus removal allowing for faster improvement of pulmonary artery pressures and SpO2 without the presence of thrombolytic complications.10 Using this approach to eliminate systemic lytic exposure from the equation provides an alternative treatment option for patients with absolute contraindications to thrombolysis. In addition to the reduced risk for major bleeding, use of mechanical thrombectomy techniques has been shown to decrease hospital costs by reducing the need for post-procedural critical care following intervention.10,11
Pages: 1 2 3 | Single Page




No Responses to “Treating Acute Pulmonary Embolism with EKOS and the Inari FlowTriever”