Evaluation of the patient with the painful shoulder can be difficult in the emergency department. The septic glenohumeral joint, while less common than infections of the knee and hip (fewer than 10 percent of cases of septic arthritis), can be often difficult to diagnose.1 Among the myriad musculoskeletal pathologies that can present with a painful shoulder, detection of a septic glenohumeral joint is critical because delay to diagnosis has been shown to allow for irreversible cartilage damage leading to functional impairment. An infected glenohumeral joint can be easily missed because classic signs and symptoms are often not present, plain film imaging does not detect a joint effusion, and classic laboratory tests are insensitive and nonspecific for septic joints.2 Also, even when a septic glenohumeral joint is suspected clinically, landmark-based aspirations can be unsuccessful. Even in the hands of experienced orthopedic surgeons, the failure rates are up to 30 percent.3 Point-of-care ultrasound allows for both an accurate method to detect the presence of a glenohumeral joint effusion and also a simplified method for reliable joint aspiration.4
Explore This Issue
ACEP Now: Vol 35 – No 06 – June 2016Procedure
1. Evaluate the nonaffected glenohumeral joint.
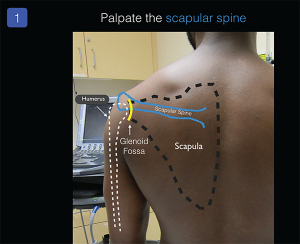
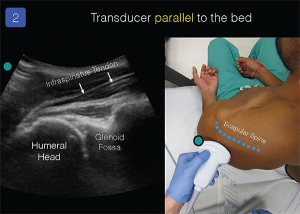
To determine the patient’s normal anatomy, obtain clear ultrasound views of the patient’s nonaffected/contralateral glenohumeral joint. For simplicity, I recommend evaluation of the posterior glenohumeral joint space (the anterior approach can be more challenging). Place the ultrasound system in front of the patient and palpate the patient’s scapular spine to identify basic surface anatomy (see Figure 1). The low-frequency (5 to 1 MHz) curvilinear transducer should be placed parallel to the bed, probe marker pointing to the patient’s left and positioned just below the scapular spine. Slowly slide the transducer toward the humeral head. A clear image of the humeral head, glenoid, infraspinatus tendon, and glenohumeral joint space will be obtained on the ultrasound screen (see Figure 2). Gentle passive or active internal and external rotation of the patient’s forearm can help novice sonographers recognize the relevant anatomy.
2. Evaluate the affected glenohumeral joint.
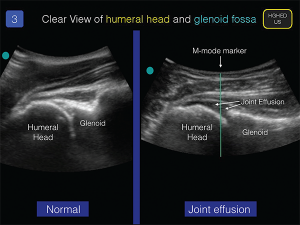
Using the same technique as detailed above, examine the affected glenohumeral joint (see Figure 3). A joint effusion will be an anechoic effusion just above the humeral head and under the synovial membrane. Exact measurements of the effusion are not useful, and the patient’s clinical evaluation, in conjunction with the ultrasound examination, should help determine the need for synovial fluid analysis.
3. Aspirate the glenohumeral joint.
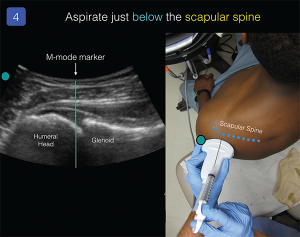
I recommend standard sterile precautions for all joint aspirations (sterile probe cover, sterile gloves, etc.). Use the M-mode marker to center the transducer over the space between the glenoid fossa and humeral head. Place a small anesthetic skin wheal at this location. With an 18–21 g, 3.5-inch spinal needle attached to a control syringe, advance the needle tip just parallel to the probe, just under the scapular spine (see Figure 4). The out-of-plane technique does not allow for clear needle visualization but offers a simplified method to enter the glenohumeral joint capsule. While advancing the needle, gently aspirate until synovial fluid is obtained.
Summary
Clinicians should be familiar with a simplified method for the ultrasonographic evaluation of the glenohumeral joint. The presence of a joint effusion on point-of-care ultrasound evaluation in the correct clinical setting will indicate the need for joint aspiration and fluid analysis. The out-of-plane posterior approach to glenohumeral aspiration allows for a simplified method for a safe and efficacious joint aspiration.
Contributors
Dennis Hsieh, MD, JD, Resident Physician, Highland General Hospital, Alameda Health System
Marcus Williams, MD, Resident Physician, Highland General Hospital, Alameda Health System
Daniel Mantuani, MD, MPH, Attending Physician, Assistant Director, Emergency Ultrasound, Highland General Hospital, Alameda Health System
Arun Nagdev, MD, Attending Physician, Director, Emergency Ultrasound, Highland General Hospital, Alameda Health System
Dr. Nagdev is director of emergency ultrasound at Highland Hospital and assistant clinical professor (volunteer) of emergency medicine at the University of California, San Francisco.
References
- Bunting L, Kuper K. Bedside washout of a septic shoulder in the emergency department: a case report. Ann Emerg Med. 2016 Feb 10 [Epub ahead of print].
- Carpenter CR, Schuur JD, Everett WW, et al. Evidence-based diagnostics: adult septic arthritis. Acad Emerg Med. 2011;18(8):781-796.
- Patel DN, Nayyar S, Hasan S, et al. Comparison of ultrasound-guided versus blind glenohumeral injections: a cadaveric study. J Shoulder Elbow Surg. 2012;21(12):1664-1668.
- Zaia BE, Soskin PN. Images in emergency medicine. Man with severe shoulder pain. Gonococcal arthritis of the shoulder. Ann Emerg Med. 2014;63(5):528.
Pages: 1 2 3 | Multi-Page





No Responses to “Ultrasound-Guided Glenohumeral Joint Evaluation and Aspiration”