Explore This Issue
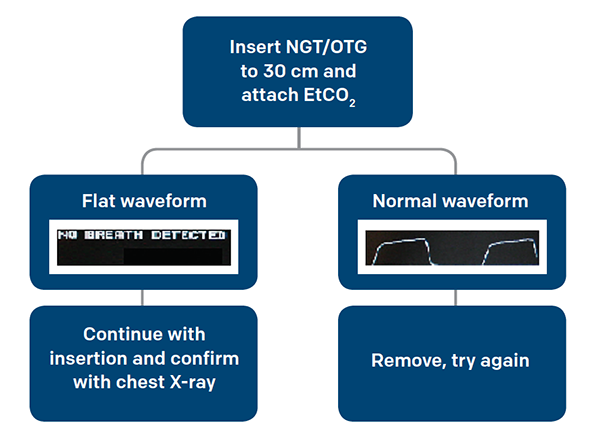
ACEP Now: Vol 35 – No 12 – December 2016Figure 2. Suggested Algorithm for Placing NGT/OGT
End-Tidal to Guide Your Next CPR
A cardiopulmonary resuscitation (CPR) is inherently a scene of chaos with many unknowns, but arguably one of most informative pieces of information, aside from presence of a pulse, is the end-tidal capnogram. End-tidal capnometry made its debut in the advanced cardiovascular life support (ACLS) guidelines in 2010, but its use in cardiac arrest can be found as far back as the 1970s.7,8 It can be used for prognostication, quality of chest compressions, correct placement of the endotracheal tube, and perhaps even the cause of the arrest.
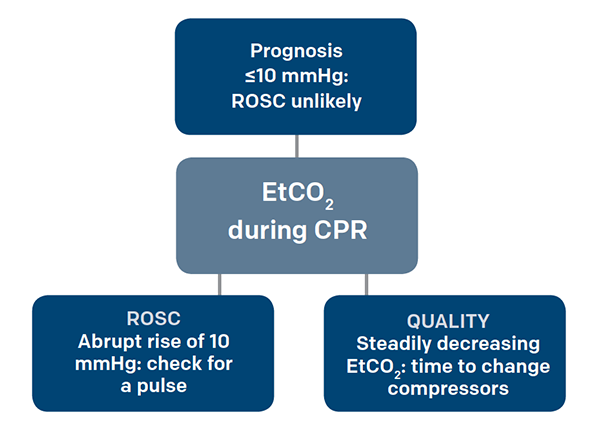
Figure 3. Using EtCO2 During CPR
When people go into cardiac arrest, they quickly become acidemic and accumulate CO2 in the blood. As CPR and ventilation begin, the CO2 is offloaded in the alveoli, expired, and subsequently sensed by the end-tidal capnometer. End-tidal CO2 has been shown to correlate with cardiac output even in low-flow states such as CPR, making it an indicator of CPR quality.9 With every increase of 10 mm in the depth of chest compressions, there is a 1.4 mmHg increase in the end-tidal value, allowing you to monitor whether the compressor is becoming fatigued and in need of relief.10 That being said, ongoing CPR should produce at least a minimal end-tidal capnogram waveform; if you see a flat capnogram, check your advanced airway for correct positioning.
The survival rates of out-of-hospital cardiac arrest are dismal, with estimations of less than 6 percent.11 End-tidal can help provide some prognostication during an active resuscitation. Having an end-tidal value less than 14.3 mmHg after undergoing 20 minutes of ACLS was predictive of not achieving return of spontaneous circulation (ROSC), with a sensitivity, specificity, positive predictive value, and negative predictive value of 100 percent.12 In a separate study where the end-tidal value at three minutes post endotracheal intubation was measured, a value 10 mmHg was also associated with a low chance of ROSC.13 In a review of 23 observational studies related to the relationship between EtCO2 and cardiac outcomes, it was emphasized that EtCO2 cannot be used as a single prognostic factor and other characteristics of the arrest must be considered; however, the correlation between low EtCO2 and low probability of achieving ROSC was again recognized. Larger organizations, such as the International Liaison Committee on Resuscitation and the American Heart Association (AHA), have agreed that low EtCO2 suggests a low probability of ROSC, with the AHA specifically mentioning values below 10 mmHg.7,14 In a more positive light, an abrupt increase of >10 mmHg in EtCO2 was associated with ROSC and shown to be a highly specific (97 percent) but not sensitive (33 percent) marker.15 During CPR, when you are typically left with very little information, end-tidal capnometry provides you with quick, reliable information that can actively guide your next resuscitation.
Pages: 1 2 3 4 | Single Page





No Responses to “Use End-Tidal Capnography for Placing Orogastric, Nasogastric Tubes, and CPR”