
The emergency department at Virginia Commonwealth University (VCU) in Richmond is one of the busiest teaching hospital emergency departments in the country. Seeing 95,000 visits a year, the adult and pediatric emergency departments were engaged in flow projects that improved their operational metrics. However, they wanted to take the adult emergency department to the next level.
Explore This Issue
ACEP Now: Vol 37 – No 01 – January 2018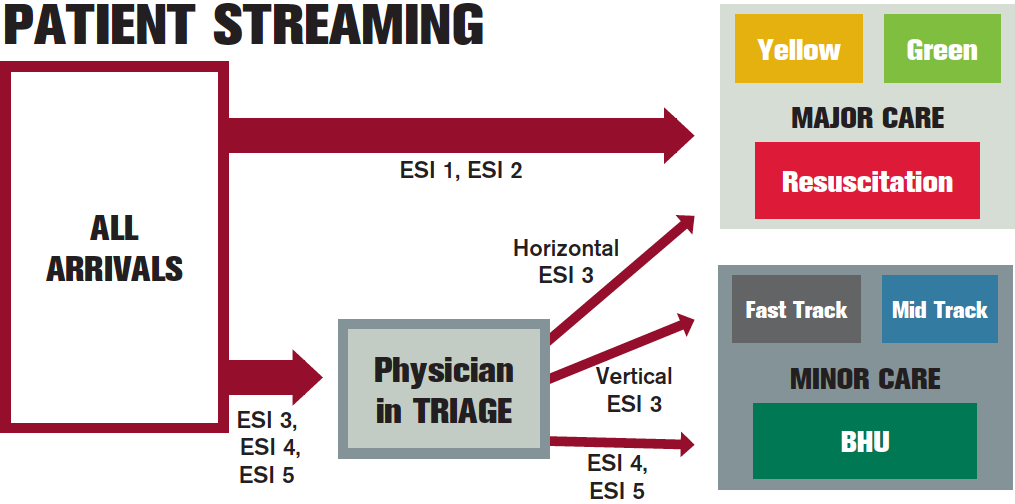
Figure 1: Vision in Action patient flow model.
The ED leadership—Harinder Dhindsa, MD, MPH; Jeremy Sauer, MD; Kathy Baker, RN, PhD; Christi Adams, RN, MSN; Anne Jackson, RN; and Jonathan Heller—had already implemented a “physician in triage” model, which reduced door-to-provider times. However, bottlenecks often meant patients went back to the waiting room, and they often eloped. In addition, the fast track, which was staffed by advanced practice providers, was underperforming, often seeing only 12 patients a day. The mid track was also not optimized. Using data-driven flow strategies, the leadership team crafted a flow model specific to its needs. It dubbed the new model “Vision in Action.”
The Plan

Figure 2: Fast track internal waiting room.
The new model (see Figure 1) has all patients screened upon arrival, and no matter if patients arrive by EMS or they were ambulatory, the greeter nurse does a quick-look Emergency Severity Index (ESI) and streams them to major care or to see the physician in triage. If the patient is assigned an ESI 1 or 2, the patient goes straight to the major care area, which includes two acute care zones and a resuscitation bay for critical patients. All other patients (ESI 3, 4, and 5) go through a physician intake area for assessment and bed placement.
The physician-streaming model includes ESI level and also anticipated length of stay in determining where the patient should go. The fast track throughput goal is to be in and out in 90 minutes, and this area is dedicated to quick, focused care without advanced imaging or complex workups. The mid track goal is to be in and out in three hours or fewer. In addition, the mid track was redesigned to involve treating patients in recliners and using fewer IV starts and more oral medications. By cleaning up the patient streams and getting the right patients to the right space and resources, new efficiencies were achieved.
Pages: 1 2 | Single Page






2 Responses to “Virginia Commonwealth University Improves Patient Flow Through “Vision in Action” Model”
January 22, 2018
Peter RizzoThere is concern of scope creep in this; why can’t the doctor at triage order tests? This established a huge bias at beginning of work up. I’d like to see if a physician at triage could only make decisions on resource management alone. However, I’m sceptical of people “wasting” that doctor as a secondary triage.
March 1, 2018
Shari WelchHello Peter,
I think the best results for physician in triage are seen when the physician is resourced to begin work-ups in triage. If all he does is determine the patient’s level of care and zone, sending patients back to the waiting room, you do not gain much in terms of time shaved off the LOS. You are playing to the metric. The only exception would be if the physician determines the stream and the patient is immediately bedded and a SWARM model employed to begin care in the back.
If you put the patient and physician together in triage for quick streaming and then send the majority back to the waiting room, you will not optimize the pIT model. You will be playing to the metric, but not shortening LOS or decreasing walkaways and patient satisfaction will not change much. That is what VCU saw. They had short D2D but high walkaways, a full waiting room and poor patient flow. When PIT was properly resourced everything changed and improved!
S