Imagine yourself in a large academic hospital in 1950s New York. You meander through the busy “accident room” and find your next patient. They’re not looking so hot. A set of vitals would help. You take out your stethoscope and your blood pressure cuff and start counting heartbeats using your wristwatch.
Explore This Issue
ACEP Now: Vol 40 – No 02 – February 2021Now return to the present day. Sitting at your workstation, you eyeball the ICU-bound patient in the bed across the room and see a reassuring set of vitals on the monitor. In the next room over, you see the same. You turn to the telemetry monitor and scroll through to ensure that you didn’t miss any arrhythmias. You quickly return to your other work with peace of mind.
Much has changed in medicine over the last 70 years. How did we come this far?
To answer this, we must return to the 1950s and what we knew—or rather didn’t know—leading into the “space race.” In preparing for travel into the inhospitable environment of space, everything that we took for granted on Earth had to be scrutinized. Would our vision, taste, smell, touch, hearing, or vestibular systems function normally? Could blood still circulate effectively in microgravity? Quaint though it may seem today, there were legitimate concerns by leading doctors at the time that humans entering microgravity would quickly develop pulmonary edema, pneumonia, or even vestibular incapacitation.1 Though it may seem trivial now, these questions were cutting-edge science at the time.
Engineers, biomedical scientists, and the astronauts themselves knew there was no guarantee of safety. Without any prior experience with humans in space, the early goals of the Mercury missions included gathering biomedical data for future missions. Telemetry instrumentation was rudimentary and confined to analog technology—there were no hard drives for storing data. So how would the ground-based teams gather data and effectively monitor astronauts’ health?
A string of remote monitoring stations established around the world whittled down the “blackout time”—no radio communication to the orbiting capsule—to no more than 10-minute spans. From these stations, the integrity of the spacecraft, its trajectory, and the health of the crew could be assessed and relayed to the next station. While orbiting Earth, Mercury astronauts’ rectal temperatures, heart rates, and respiratory rates were transmitted by radio to each passing monitoring site. They were also interviewed via radio by medical monitors to assess their cognition and any self-reported symptoms.2 Reassuring data were collected in this manner, but the technical difficulties underscored the need for more reliable monitoring.
With planning under way for the Gemini and Apollo programs, a new company, Spacelabs Medical, Inc., was subcontracted to help develop better telemetry monitoring systems. The technology produced by this partnership paved the way for the modern telemetry systems we now use in hospitals around the world. Respiratory rate—previously measured by a thermistor situated near the mouth in crew helmets—could now be reliably calculated using electrical impedance of the thorax via ECG electrodes (ie, leads). An automated blood pressure cuff outfitted with microphones could independently detect the systolic and diastolic Korotkoff sounds. Development of signal conditioners to mitigate signal noise also improved the fidelity of ECG, blood pressure, and respiratory rate readings, leading to more accurate and extensive data collection.3,4
These improvements laid the foundation for the biomedical research of subsequent programs like Skylab and Spacelab. By the late 1960s, having proven their mettle in space, these technologies started being implemented here on Earth in hospitals across the country. The benefit of continuous, remote patient monitoring spread rapidly. The standard use of telemetry systems soon became a given in hospitals worldwide. Decades of further innovation and refinement have resulted in the systems we know well today. (For example, we no longer have microphones in our automatic cuffs!)
But what comes next? Wireless telemetry? We’ve all experienced the frustration of preparing a patient for transport and all of the wires and IV lines that must be repeatedly disentangled. Carré Technologies of Montreal, working in conjunction with the Canadian Space Agency, may have the answer to our ongoing tangle torture thanks to its recently developed Bio-Monitor telemetry shirt.
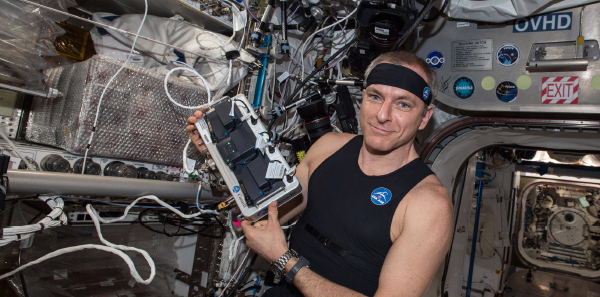
Astronauts aboard the International Space Station are already using the Bio-Monitor, known as Astroskin. Astroskin is a shirt that is capable of wirelessly transmitting vital signs, including heart rate, ECG readings, blood pressure measurements, oxygen saturation, temperature, and respiratory rate.5 While the technology is not yet ready for hospital use, it is already being used in a variety of ground-based applications, including monitoring high-performance athletes in training. Other companies are developing similar wireless products. It’s only a matter of time until we have these technologies in our hospitals. With the aerospace industry continually pushing the technological envelope for space- and ground-based applications, we will continue to reap the benefits of what is learned, applying these innovations to caring for our patients with less hassle and increased safety.
For more information, check out the Aerospace Medicine Section.
Pages: 1 2 | Single Page



No Responses to “We Can Thank the Space Race for Patient Monitoring Technologies”