One example of this is connected inhalers from Propeller Health. By creating a connected inhaler, patients with asthma and chronic obstructive pulmonary disease have much better objective data regarding their usage. Prior to this, at best, patients would keep usage diaries to share with providers, but more commonly, it was just a vague estimation of use. Now, definitive data on frequency of use, time of day, and weather can be acquired and correlated. One may also be able to determine geographic areas that seem to trigger an increased use of medication. Not only do these data allow the user to be more actively involved in the management of the disease, but they also create a novel way in which the patient can engage with a health care provider. As emergency physicians, we can expect to be shown the app or printouts that summarize the data captured by a connected inhaler.
Explore This Issue
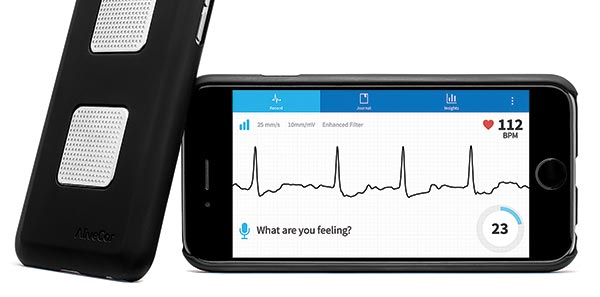
ACEP Now: Vol 36 – No 01 – January 2017AliveCor’s Kardia (~$125) has been on the market now for a few years and provides a single-lead ECG when the user puts fingers from each hand on the back of an integrated mobile phone case. The Food and Drug Administration (FDA) approved machine learning algorithms that can help differentiate atrial fibrillation from normal sinus rhythm. Large data sets are available to be shared with emergency physicians upon arrival to the emergency department. Even more compelling is the Kardia wristband, which is pending FDA 510(k) clearance. This will take the technology one step further by providing passive, continuous cardiac rhythm monitoring. AliveCor claims that the device improves outcomes, reduces cost, increases workflow productivity, and deepens clinician-patient relationships. On Sept. 8, 2016, AliveCor announced a partnership with Omron that integrates blood pressure readings from Omron devices (~$65) with the Kardia app, creating a more robust data set.
Products like MedMinder have reported functionality that will take medication reconciliation to the next level, certainly something we may come across in the emergency department. There are alerts, texting functionality, and online reports that emergency physicians may be assessing.
Medication compliance is a huge issue in medicine. A number of entrepreneurs are attempting to tackle this by better controlling distribution of medications. There are a number of companies that have developed pill-dispensing systems, some of them attached to the pill bottle itself. Appropriate medication dosing can be accurately adhered to, ensuring that people take their medication and that people don’t overdose. Products like MedMinder have reported functionality that will take medication reconciliation to the next level, certainly something we may come across in the emergency department. There are alerts, texting functionality, and online reports that emergency physicians may be assessing. A step further are digestible digital medicines with sensors embedded in pills from the company Proteus Digital Health. It has developed an ingestible sensor the size of a grain of sand that, when ingested, sends a recordable signal to a patch that the patient wears on the torso. These data are transmitted to the patient’s mobile device and up to the cloud, where they sit in a portal that allows providers to access and review a patient’s medication administration history. This takes medication compliance from subjective data (self-reporting) to objective data (sensor reporting), thereby optimizing adherence and patient outcomes.
Pages: 1 2 3 | Single Page



One Response to “Wearable Health Care Technology, Devices that Emergency Physicians Need to Know About”
September 15, 2017
KevinC-MDYou can buy NIBP, pulse ox, finger stick glucose, pregnancy test*, and dip UA* at Walgreens. The cost to produce (albeit not license) a wearable multilead ECG is within most patient’s discretionary healthcare spending. While we agonize over all the false positives and worried well, good analytics/AI could greatly help in both detecting serious injury or excluding things like unstable angina.
But, it is totally a pipe dream, or bad trip.
The electronic health record systems in use in the vast majority of acute care hospitals are incapable of even the most simple standard-based information exchange. These IoT devices will drive up consumer (what we call patient’s) expectations (“Its in my FitBit”) and create substantial investor/regulator/end-user resentment.
As emergency physician’s we need to stop accepting the antiquated (largely unstudied, if you use a commercial system), and potentially dangerous impediments to safe and efficient patient care.
Technology can be a great boon. What has been shoveled to us, however, is not. Realistic at home data collection (which should include additional low hanging fruit as daily weight and spirometer results) likely can help PCPs and EPs detect and abort early stage disease.
Without decent emergency department information systems (EDIS) and electronic health record system (EHRS), however, we are stuck.
While administrators may be patting themselves on the back (or wringing their hands over the exorbitant sunk costs) for “successfully deploying” what amounts to a crappy documentation(word processing?) and ordering (a lot like emailing tasks with circa 1995 MS Outlook) system, the “proven” benefits fail to manifest (almost all shown using home grown, typically physician directed/engineered), and productivity takes a permanent record.
Want this 21st century in-put? Let’s force the issue and demand a 21st century EDIS!
*Tests, like fecal occult blood and wet preps, we no longer are smart enough to do in the ED (but that is another issue).