Explore This Issue
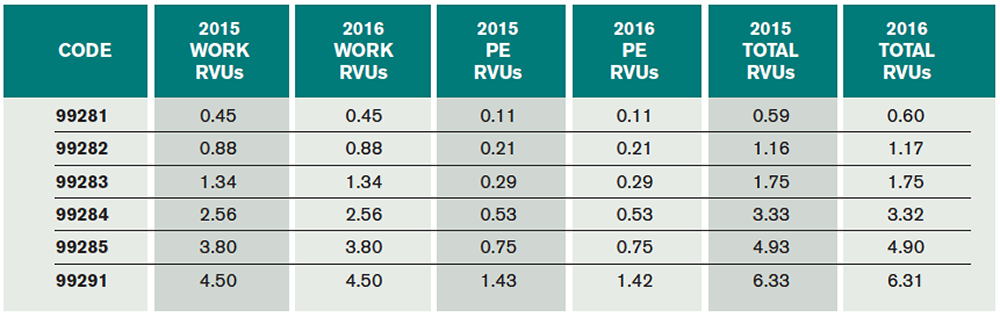
ACEP Now: Vol 35 – No 01 – January 2016(click for larger image) Table 3. 2016 ED E/M RVUs 99281–99285
Critical Care Services
Critical care services were also revalued as part of the Final Rule and benefited from a small increase (see Table 4).
Physician Quality Reporting System
PQRS continues for 2016. Groups not reporting PQRS measures in 2016 will receive a 2 percent penalty assessed against their 2018 Medicare allowables. Additionally, failing to satisfy 2016 PQRS reporting requirements would trigger an additional 4 percent penalty for most groups under the VBM program for a total penalty of 6 percent in 2018.
For 2016, satisfactory PQRS reporting requires at least nine measures, involving three National Quality Strategy domains, for at least 50 percent of the Medicare part B patients during the year. Additionally, the 2015 requirement for reporting on a cross-cutting measure continues for 2016.
The predominant 2016 potential CMS ED PQRS measures typically applicable to ED providers are listed in Table 5. There are also three new measures related to head CT utilization, including head CT for adult blunt head trauma, head CT use in the pediatric population, and use of neuroimaging in patients with a primary headache.
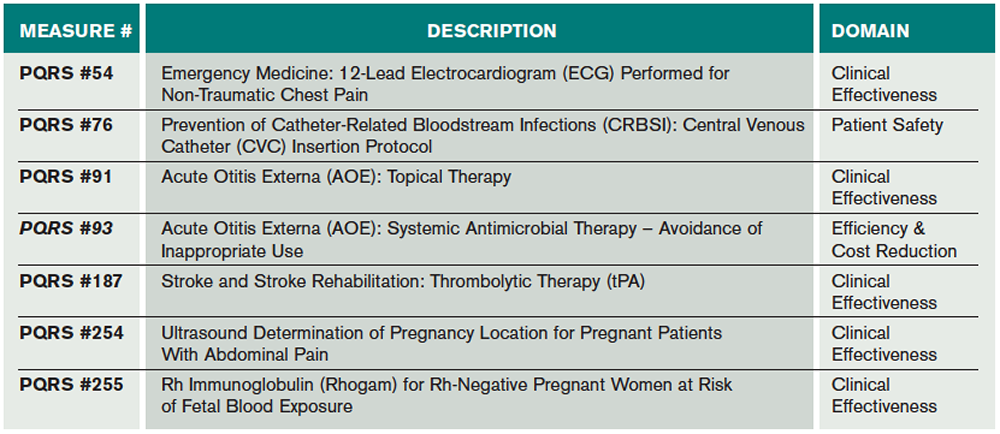
(click for larger image) Table 5. Predominant 2016 Potential CMS ED PQRS Measures Typically Applicable to ED Providers
2016 Value-Based Payment Modifier
The Affordable Care Act requires CMS to apply a VBM to physician payments for all providers by 2017. CMS has been gradually phasing in the VBM program. For 2016, the VBM carries a potential penalty of 4.0 percent for groups of 10 or more providers (eligible providers include all physicians and advanced practice providers, full time and part time). The VBM penalty will be applied to 2018 payments based on 2016 dates of service. The VBM penalty will be avoided if at least 50 percent of the providers within a group satisfy the minimum PQRS reporting requirements in 2016.
CMS is also continuing the VBM scoring methodology, which looks at both cost and quality scoring for individual providers and groups. Failing to meet the PQRS reporting requirements would trigger an automatic 4 percent penalty under the VBM program (see Table 6 for a summary of PQRS penalties). Groups satisfying PQRS reporting go on to the quality-tiering step and will be graded as below average, average, or above average and have the potential to earn a small bonus. Importantly, as MIPS takes over in 2019, VBM is being phased out after 2018.
Pages: 1 2 3 | Single Page






No Responses to “What Emergency Physicians Need to Know about the 2016 CMS Fee Schedule”