
The 2019 Medicare Physician Fee Schedule Proposed Rule was released on July 12, 2018, and it includes significant proposed changes from the Centers for Medicare and Medicaid Services (CMS) relevant to emergency medicine. ACEP has submitted robust commentary on it. The Final Rule should be released in November and go into effect Jan. 1, 2019.
Explore This Issue
ACEP Now: Vol 37 – No 09 – September 2018Here are some emergency medicine–related highlights from the Proposed Rule.
RVU Remains Stable
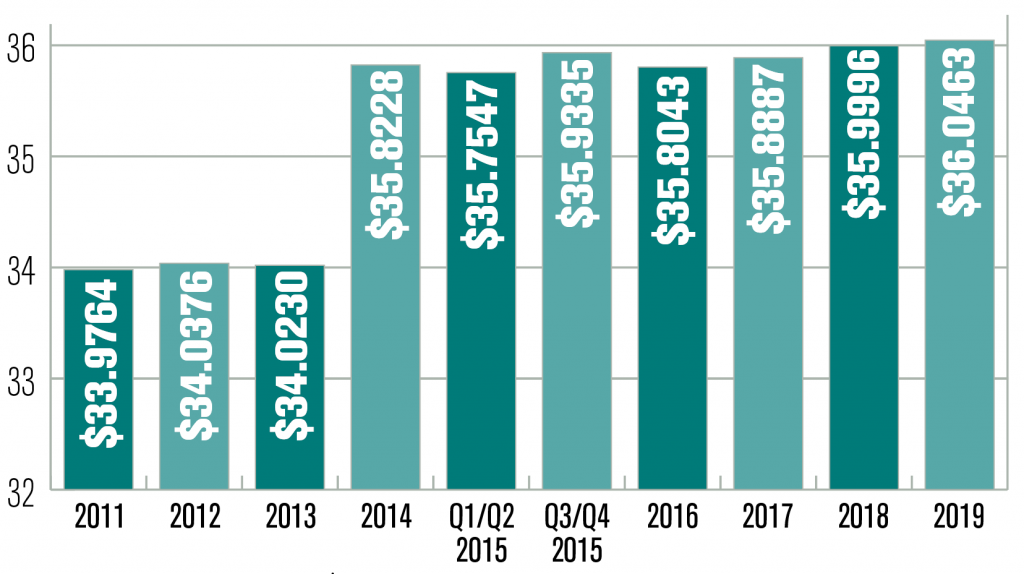
Each year, based on several technical formulas, CMS publishes the Medicare reimbursement rate per relative value unit (RVU, ie, the conversion factor). Many private payers then incorporate the Medicare changes when considering their own rates, so this conversion factor has far-reaching economic implications.
The proposed 2019 conversion factor of $36.0463 represents a slight increase from 2018’s $35.9996. Following a low point in 2011, the conversion factor has generally increased and is no longer governed by the flawed Sustainable Growth Rate formula (see Figure 1).
The RVU Value of ED Codes
At the end of last year, the 2018 Physician Final Rule highlighted concerns that emergency department evaluation and management (E/M) services may be undervalued:
“We received information suggesting that the work RVUs for emergency department visits did not appropriately reflect the full resources involved in furnishing these services. We agree with the majority of commenters that these services may be potentially misvalued given the increased acuity of the patient population. As a result, we look forward to reviewing the RUC’s recommendations regarding the appropriate valuation of these services for our consideration in future notice and comment rulemaking.”
ACEP’s Relative Value Update Committee recently presented the ED E/M codes (99281–99285) that make up 83 percent of our RVUs for valuation by the Relative Value Scale Update Committee (RUC). Although the RUC’s deliberations remain confidential, I can say the ACEP committee mounted vigorous arguments defending the increase in the acuity of our patients, and CMS is currently considering the RUC’s recommendations.
ED Codes Not Affected
Toward the end of 2018, CMS expressed dissatisfaction with the widely applied 1995 Documentation Guidelines for Evaluation and Management Services, stating they may not reflect today’s more electronic clinical documentation processes:
“The guidelines have not been updated to account for significant changes in technology, especially electronic health record (EHR) use, which presents challenges for data and program integrity and potential upcoding, given the frequently automated selection of code level. In the near-term, it may be possible to eliminate the current focus on details of history and physical exam, and allow MDM [medical decision making] and/or time to serve as the key determinant of E/M visit level.”
Pages: 1 2 3 | Single Page






No Responses to “What’s in the 2019 Medicare Physician Fee Schedule Proposed Rule?”