
Explore This Issue
ACEP Now: Vol 42 – No 07 – July 2023Treatment in patients
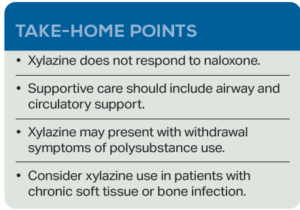
Xylazine should be considered in all patients who present with history of injection drug use and chronic wounds. Initial stabilization includes airway management and circulatory support. Currently, there is no FDA-approved pharmacotherapy for either the reversal of xylazine in humans or the management of withdrawal. Typically, xylazine is mixed with fentanyl. While naloxone can treat fentanyl overdose, overdose symptoms may persist when xylazine is involved.
Workup may include metabolic panel, complete blood count, and imaging in cases where trauma or infection occur. Xylazine is not detected by routine toxicologic studies. Xylazine-induced skin ulcers typically begin as a blackened eschar that progresses to a cribriform appearance.10 The wounds are purulent and often polymicrobial. Many of these infections require hospitalization with intravenous antibiotics and surgical debridement. However, xylazine withdrawal is often so miserable that patients are at risk of leaving the hospital against medical advice before treatment is completed.
 Isha Joshi (@ISHAJOSHIII) is a third-year medical student at Penn State College of Medicine in Hershey, Pa. Prior to medical school, she received her MBA in Healthcare Management and currently works on health policy and outcomes-based research.
Isha Joshi (@ISHAJOSHIII) is a third-year medical student at Penn State College of Medicine in Hershey, Pa. Prior to medical school, she received her MBA in Healthcare Management and currently works on health policy and outcomes-based research.
 Dr. Marco is professor of emergency medicine at Penn State Health Milton S. Hershey Medical Center and the associate editor of ACEP Now.
Dr. Marco is professor of emergency medicine at Penn State Health Milton S. Hershey Medical Center and the associate editor of ACEP Now.
 Dr. Lubin is a professor of emergency medicine and public health sciences and the program director for the MD/MPH dual degree program at the Penn State College of Medicine in Hershey, PA, where he is also the vice chair of research for the department of emergency medicine at the Penn State Health Milton S. Hershey Medical Center.
Dr. Lubin is a professor of emergency medicine and public health sciences and the program director for the MD/MPH dual degree program at the Penn State College of Medicine in Hershey, PA, where he is also the vice chair of research for the department of emergency medicine at the Penn State Health Milton S. Hershey Medical Center.
References
- Friedman J, et al. Xylazine spreads across the US: A growing component of the increasingly synthetic and polysubstance overdose crisis. Drug and Alcohol Dependence. 2022;233:109380.
- Alexander RS, et al. Xylazine and overdoses: Trends, concerns, and recommendations. Am J Public Health. 2022;112(8):1212-1216.
- Love JS, et al. Opioid overdoses involving xylazine in emergency department patients: a multicenter study. Clin Toxicol (Phila). 2023 Mar;61(3):173-180.
- US Department of Justice, Drug Enforcement Administration. The Growing Threat of Xylazine and its Mixture with Illicit Drugs: DEA Joint Intelligence Report. DEA Product Number DCI-DIR-001-23. Available here. Published online October, 2022. Accessed June 16, 2023.
- Reyes JC, et al. The emerging of xylazine as a new drug of abuse and its health consequences among drug users in Puerto Rico. J Urban Health. 2012;89(3):519-26.
- Ruiz-Colón K, et al. (2014). Xylazine intoxication in humans and its importance as an emerging adulterant in abused drugs: A comprehensive review of the literature. Forensic Sci Int. 2014;240:1-8.
- Capraro AJ, et al. (2001). Severe intoxication from xylazine inhalation. Pediatr Emerg Care. 2001;17(6):447-8.
- Gupta R: Xylazine – Medical and public health imperatives. N Engl J Med. 2023; 15;388(24):2209-2212.
- Rodríguez N, et al. GC-MS confirmation of xylazine (Rompun), a veterinary sedative, in exchanged needles. Drug and alcohol dependence. 2008;96(3):290–293.
- Malayala SV, et al. Xylazine-induced skin ulcers in a person who injects drugs in Philadelphia, Pennsylvania, USA. Cureus. 2022;14(8):e28160.
Pages: 1 2 3 | Single Page





No Responses to “Xylazine: An Emerging Threat”