Intermountain Medical Center, flagship hospital of the health system by the same name, sits nestled along the Wasatch Mountains in Utah. It is a bright, modern urban medical center, a tertiary teaching hospital, a transplant center, and a Level One Trauma Center. The emergency department sees 90,000 visits per year in its 75 beds. In short, it has the characteristics of an emergency department that should struggle with efficiency and performance.
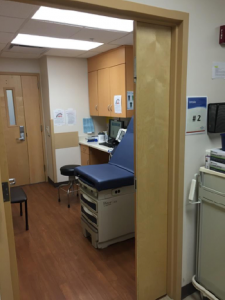
Intake room. (Image courtesy of Adam Balls, MD, and Brian Oliver, MD.)
However, in 2015, it was already performing very well compared to emergency departments in its cohort. Overall median lengths of stay (LOS) were 207 minutes, door to provider (Door to Doc) times were consistently under 30 minutes, and the left without being seen (LWBS) rate was 2.4 percent. By comparison, according to the Emergency Department Benchmarking Alliance, the median overall LOS for hospitals of this size is 227 minutes, Door to Doc is 32 minutes, and LWBS is 3.1 percent. Despite very strong operational metrics, the quality-minded doctors (Utah Emergency Physicians) led by the director and assistant director, Adam Balls, MD, and Brian Oliver, MD, were tasked with reengineering their ED flow. In preparation for the current changing health care imperatives, the hospital leadership wished to open up an observation unit within the emergency department. The only way this would be possible would be to put physicians in triage and move to a vertical flow model, no longer bedding every patient. This model has also been shown to deliver improvements in the efficiency of care delivered to lower-acuity patients.

Results waiting area. (Image courtesy of Adam Balls, MD, and Brian Oliver, MD.)
Adapting a version of Jody Crane’s AcceleratED flow model (which is a version of the team triage model that keeps patients vertical and brings the staff and supplies to patients), the ED leaders reinvented their patient flow and workflow. The concept is that many patients can be completely evaluated and treated without occupying an ED bed. They arrive and remain ambulatory, and resources are brought to them. The model involves careful selection of which patients can be appropriately treated in this manner. This was a project that turned on a dime. With a one-week rapid-cycle testing phase, the project was off and running. Moving to a vertical patient flow model is one of the easiest improvements to introduce in the emergency department with regard to implementation.
Pages: 1 2 3 | Single Page






One Response to “Intermountain Medical Center in Utah Improves Efficiency, Performance with Vertical Flow Model”
April 25, 2017
Anna FraserHi there,
Where did you get the Door to Doc, LOS and LWBS statistics from? Do you have a valid source you can pass on to me?
Regards,
Anna