The Case
A 24-year-old male presents to the ED late Saturday night after leaving the local watering hole. One may say he had a few too many, but according to the patient, he was just “minding his own business” when he was “sucker punched” in the right eye. The patient now is unable to see out of his right eye. On exam, you find severe periorbital edema, decreased visual acuity, and an afferent pupillary defect (Marcus-Gunn) in the right eye. A CT of the head and maxillofacial bones is performed, which is negative for intracranial hemorrhage or retrobulbar hematoma. After fluorescein staining, you check the intraocular pressure only to find it to be 45 mm Hg. As an emergency physician, you begin to have flight of ideas: Is there any indication to perform a lateral canthotomy without a retrobulbar hematoma? Visualization to perform the procedure is a problem due to edema. Is there a trick to improve visualization and prevent iatrogenic globe rupture?
Explore This Issue
ACEP Now: Vol 34 – No 03 – March 2015Indications for Lateral Canthotomy
Emergency physicians are commonly taught that the indication for lateral canthotomy and inferior cantholysis is acute trauma with a retrobulbar hematoma causing an increase in the intraocular pressure. While this is a classic example, and an appropriate indication to dust off the iris scissors, it is far from the only reason to perform this potentially vision-saving procedure.1–5 Orbital compartment syndrome (OCS) is an ophthalmologic emergency that, unfortunately, is on the rise due to increasing use of antiplatelet and anticoagulant medications.1 In turn, emergency physicians across the country are going to be called upon more frequently to perform a decompression of the orbit in a timely fashion. Studies suggest permanent vision loss can be seen in as little as 30 minutes once the intraocular pressure (IOP) threshold is met.2 Prompt recognition and familiarity with the indications to perform a lateral canthotomy are crucial to improve the chances of preserving the patient’s vision. This begets two questions: When do you perform a lateral canthotomy? And does releasing the inferior tendon from the bony orbit improve outcomes?
When discussing outcomes of a lateral canthotomy, most studies look at intraocular pressure as the primary outcome of the trial. With regard to IOP, a 2009 article by Lima et al showed a greater reduction in intraocular pressure was achieved by lateral canthotomy and cantholysis (30.4 mm Hg) compared with canthotomy (14.2 mm Hg) or cantholysis (19.2 mm Hg) alone, answering the age-old question of whether inferior cantholysis is helpful.1
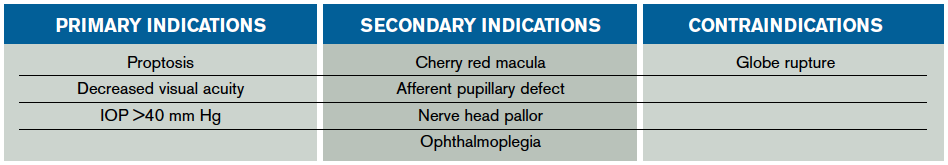
The indication to perform a lateral canthotomy does not change regardless of the underlying cause. Astute emergency physicians will attempt to uncover the cause of OCS in the setting of multiple etiologies not commonly mentioned in texts or the literature. The commonly cited retrobulbar hematoma is only one of many underlying etiologies requiring emergent decompression. Others include orbital cellulitis; foreign material; orbital edema (trauma, massive fluid resuscitation, thermal injuries); orbital emphysema; intraocular injections; postoperative complications from periorbital surgery; caustic injuries; or retrobulbar hemorrhage from thrombolysis, sickle cell disease, or leukemia.1 In the setting of any of the aforementioned injuries or disease processes, physicians should look for primary or secondary indications to perform a lateral canthotomy to preserve vision. Primary indications include proptosis and decreased visual acuity or IOP >40 mm Hg, while secondary indications are more subjective findings such as an afferent pupillary defect (APD), ophthalmoplegia, nerve head pallor, or a cherry red macula (see Table 1).3
Physicians should look for any sign of orbital compartment syndrome and immediately move forward with a lateral canthotomy once the decision is made because “time is vision.”
A Paper Clip and a Morgan Lens: Tricks for Lateral Canthotomy
Performing a lateral canthotomy is a heroic—yet stressful—potentially vision-sparing procedure all emergency physicians prepare for and yet rarely perform. When the time comes to perform a lateral canthotomy, emergency physicians may play back Roberts & Hedges’ Clinical Procedures in Emergency Medicine in their mind to carry out each step. It seems so simple, almost mindless, to cut the lateral canthal tendon—that is, until you add in the periorbital edema and chemosis that impairs visualization for the procedure. While there are several strategies to help improve visualization, and therefore success rates, using a paper clip bent into a hook to displace the eyelid for the procedure is a safe adjunct and utilizes equipment easily found in any ED.
Any time emergency physicians perform a procedure such as a lateral canthotomy, providers experience a surge of endogenous catecholamines leading to tachycardia, perspiration, and even tremors. With one slip of the hand, the iris scissor point can accidentally penetrate the lateral aspect of the globe, leading to an iatrogenic globe rupture. What if this fear could simply be put to rest by a device readily found in all EDs? A Morgan lens can be placed on the cornea prior to the procedure to act as a shield to prevent iatrogenic globe rupture.
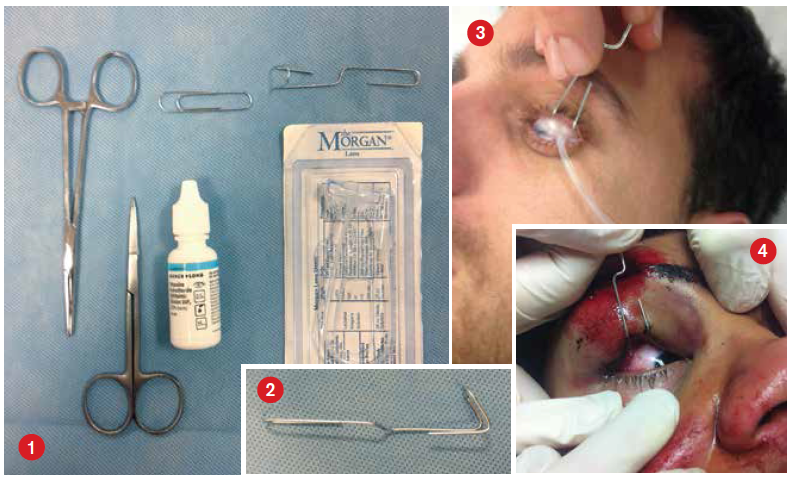
Equipment (see Figure 1)
- One Morgan lens
- Medium-sized paper clip
- Topical anesthetic ophthalmic drops (eg, tetracaine)
- Standard equipment for lateral canthotomy and cantholysis
Technique
- Place the patient in a comfortable supine position at a height suitable for you to perform the lateral canthotomy and cantholysis.
- Bend the medium-sized paper clip into a hook with a handle (see Figure 2) that can be used to retract the eyelids for the procedure (see Figure 3). (Paper clips can be used for both upper and lower eyelids if deemed necessary for visualization.)
- Place two drops of topical anesthetic ophthalmic drops into the eye in which you will be performing the lateral canthotomy. (Caution: Do not use the anesthetic drops prior to checking the pH if the underlying etiology is a caustic exposure.)
- Place the Morgan lens into the affected eye prior to the start of the lateral canthotomy and cantholysis (see Figure 3). No irrigation fluid is necessary.
- Have an assistant use the paper clip to hook the eyelid and retract it to improve exposure and visualization during the procedure (see Figure 4).
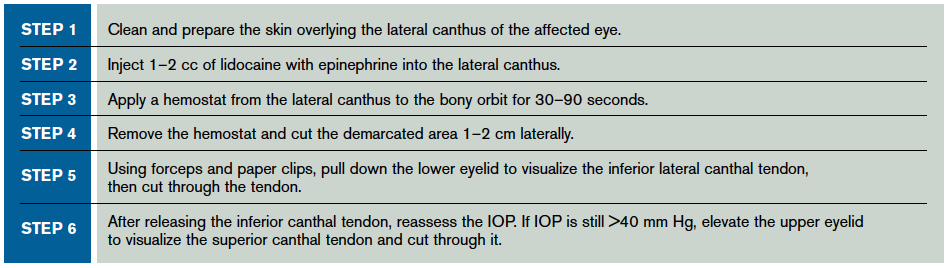
- Perform the lateral canthotomy and cantholysis (see Table 2).
Patient Selection
This technique is typically applicable to cooperative pediatric and adult patients who will allow the insertion of a Morgan lens onto their cornea. In the case of an uncooperative patient, procedural sedation may be used in order to successfully and safely perform the procedure. The use of a paper clip and Morgan lens remains very valuable after procedural sedation and prior to the onset of the lateral canthotomy.
Caution
A 2002 Canadian Journal of Emergency Medicine article by McInnes and Howe reports several complications of lateral canthotomy, ranging from minor postoperative bleeding and infection to the most-feared complication, iatrogenic globe rupture.3 Our proposed technique for performing a lateral canthotomy and cantholysis protects against iatrogenic globe rupture. However, it potentially increases the risk of corneal abrasions due to placing the Morgan lens over the cornea. In a risk-benefit analysis, most providers would opt for a corneal abrasion as opposed to an iatrogenic globe rupture. The Morgan lens also provides a sense of comfort by having a physical barrier present during this critical procedure and period of high stress.
Caution should be exercised when placing topical anesthetic drops into the eyes of patients who have suffered a caustic injury. A litmus-paper test to determine the pH prior to placing the drops should be performed because topical anesthetic drops, in theory, could lower the pH, leading to worsening injury or permanent vision loss.4
 Dr. McGovern is an emergency medicine resident at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
Dr. McGovern is an emergency medicine resident at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
 Dr. McNamee is chief resident of the emergency medicine residency at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
Dr. McNamee is chief resident of the emergency medicine residency at St. Joseph’s Regional Medical Center in Paterson, New Jersey.
 Dr. Patel is associate program director, emergency medicine, at St. Joseph’s.
Dr. Patel is associate program director, emergency medicine, at St. Joseph’s.
References
- Lima V, Burt B, Leibovitch I, et al. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009;54(4):441-449. Oester AE Jr, Fowler BT, Fleming JC.
- Oester AE Jr, Fowler BT, Fleming JC. Inferior orbital septum release compared with lateral canthotomy and cantholysis in the management of orbital compartment syndrome. Ophthal Plast Reconstr Surg. 2012;28(1):40-43.
- McInnes G, Howes D. Lateral canthotomy and cantholysis: a simple, vision-saving procedure. CJEM. 2002;4(1):49-52.
- Bord SP, Linden J. Trauma to the globe and orbit. Emerg Med Clin North Am. 2008;26(1):97-123.
- Carrim ZI, Anderson IW, Kyle PM. Traumatic orbital compartment syndrome: importance of prompt recognition and management. Eur J Emerg Med. 2007;14(3):174-176.
Pages: 1 2 3 4 | Multi-Page





2 Responses to “Tips for Relieving Increased Intraocular Pressure”
April 5, 2015
John Patrick MDA more accurate title for this would be “Tips for Relieving Increased Intraorbital Pressure” or “Tips for Relieving Secondarily Increased Intraocular Pressure”
April 9, 2015
neat trick: morgan lens for lateral canthotomy | DAILYEM[…] References: ACEP Now article + picture from article […]