
When I was a young recruiter in New York City, I spent many a summer weekend in the Hamptons, a string of small towns and hamlets along the eastern tip of Long Island. On any given Friday afternoon, as trains from Penn Station crammed with vacationers and packed like sardines with day-trippers in standing-room-only accommodations, the cacophony of voices and metal wheels shrieking against the rails was deafening. On one particular trip, there was a lull in the conversation, and I distinctly heard a lone voice exclaim, “Do you think there will be jobs when we get to America?” Of course, laughter exploded.
Explore This Issue
ACEP Now: Vol 40 – No 10 – October 2021For the first time in the 32 years that I’ve worked in the emergency medicine arena, residents are asking, “Do you think there will be jobs when we get to graduation?” But this time, no one is laughing. The COVID-19 pandemic wreaked havoc on the specialty, with emergency department census levels dipping 42 percent overall early in the pandemic1—and as much as 70 percent in some places. Physicians saw clinical hours cut back and salaries reduced; some were even laid off. The number of job opportunities for physicians dove well under 50 percent of 2019 levels, and some 2021 graduates left residency without a job. More than 75 percent of jobs were open to primary care boarded physicians, and there are reports of some employers replacing physicians with physician assistants and nurse practitioners to keep costs down.
So where is this pandemic train taking us?
In May 2021, I surveyed employers representing approximately 32 percent of the 8,600 emergency departments in the country and received about a 70 percent response rate. Employers ranged from small democratic groups to large national groups and included a strong percentage of teams employed directly by hospitals. The survey focused on both the past 2020–2021 and the upcoming 2021–2022 hiring seasons. Below are some highlights from these employers.
Current Workforce
Part one of the survey addressed current workforce status: 63 percent of respondents stated that their workforce numbers were the same as pre-COVID levels, and 37 percent reported their workforce was smaller. Staff reduction percentages ranged from 8 to 40 percent, with an average of 16 percent. Slightly more than 69 percent of employers have cut back on physician clinical hours, ranging from 5 to 30 percent, with an average of 15 percent.
 On the compensation front, only 21 percent of respondents reported salary cuts for physicians, ranging from 5 to 20 percent, with an average of 12.5 percent. Some employers took steps to prevent cuts, including one large national group that had its leadership team take cuts so its physicians wouldn’t have to bear the brunt of the financial burden. The survey also asked about cuts to advances for new hires. Responses showed 68 percent experiencing no change and 32 percent cutting as much as half of the value of signing bonuses, loan forgiveness, relocation packages, and resident early sign-on stipends.
On the compensation front, only 21 percent of respondents reported salary cuts for physicians, ranging from 5 to 20 percent, with an average of 12.5 percent. Some employers took steps to prevent cuts, including one large national group that had its leadership team take cuts so its physicians wouldn’t have to bear the brunt of the financial burden. The survey also asked about cuts to advances for new hires. Responses showed 68 percent experiencing no change and 32 percent cutting as much as half of the value of signing bonuses, loan forgiveness, relocation packages, and resident early sign-on stipends.
Next, the survey asked employers the percentage of primary care trained physicians on their workforce. Responses indicated higher levels than the pre-COVID period, with 58 percent having primary care boarded physicians, ranging from 5 to 100 percent of their staff, with an average of 32 percent of their workforce. Finally, the survey asked if employers had replaced any physicians with physician assistants and nurse practitioner—not a single employer who responded to the survey had done so.
Hiring Plans
Part two of the survey focused on the then-upcoming 2021–2022 hiring season, which is now under way. In pre-COVID days, the specialty’s primary web-based job search site, EDPhysician.com, averaged 1,700 jobs on any given day. During COVID and as recent as July 2021, that number dipped dramatically to about 500 listings.
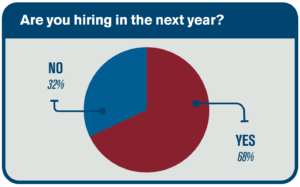 Who is hiring? Of all respondents, 68 percent will be hiring, while 32 percent, composed primarily of small emergency medicine groups or single hospital employers, will not. Large national groups anticipated hiring just over 1,000 physicians, while the smaller employers hoped to add a collective 150 new physicians. Of those who are hiring, 31 percent will see an increase from the pre-COVID workforce, while 47 percent will stay the same.
Who is hiring? Of all respondents, 68 percent will be hiring, while 32 percent, composed primarily of small emergency medicine groups or single hospital employers, will not. Large national groups anticipated hiring just over 1,000 physicians, while the smaller employers hoped to add a collective 150 new physicians. Of those who are hiring, 31 percent will see an increase from the pre-COVID workforce, while 47 percent will stay the same.
Finally, the survey asked when employers anticipated beginning the recruitment process. Just over half of employers (52 percent) planned to open for applications in July, 10 percent planned to initiate hiring in September, and 6 percent will start interviewing in January 2022. Of those who will be hiring, 62 percent will not consider primary care boarded candidates.
Compensation
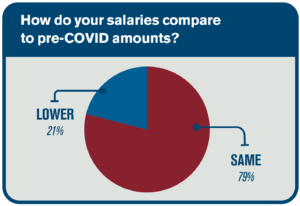
Part three of the survey focused on compensation levels for this season’s new hires. Of employers that are hiring, 79 percent will retain pre-COVID compensation levels, while 21 percent will experience a compensation level as much as 20 percent lower. As for up-front incentives, 50 percent of employers will offer the same bonuses as pre-COVID levels; the other half will lower the perks they offer. Most of the cuts will be from sign-on bonuses, with employers either reducing the amount or eliminating these deal sweeteners altogether.
Market Outlook
Finally, the survey inquired about employers’ other concerns for the emergency medicine job outlook. A representative from a large national physician owned group replied, “Rural, less desirable locations will always be in shortage. Hospitals will have to incentivize providers to live and work in those locations in the form of money. If they do entice with dollars, unfortunately, turnover in those areas will be an ongoing problem.”
The emergency department chief of a multisite Midwestern group stated, “I am concerned with cost cutting by hospitals by reduction of board-certified emergency physicians overall and movement toward mid-level providers.”
The representative of another large national group mentioned factors that excite him: “It’s about the value of the training we get. We really have the skills to care for a broad scope of patients from critical care to jail medicine. There continues to be lots of opportunity in emergency medicine.”
 And the chief of a large medical center emergency department opined that he was concerned about multiple factors: “The increase of private-equity ownership of EM practices, the increase in emergency medicine programs that are started for the purposed of creating cheap labor, and the replacement of physicians with APPs as it relates to private equity.”
And the chief of a large medical center emergency department opined that he was concerned about multiple factors: “The increase of private-equity ownership of EM practices, the increase in emergency medicine programs that are started for the purposed of creating cheap labor, and the replacement of physicians with APPs as it relates to private equity.”
Conclusion
The specialty of emergency medicine is in recovery mode, and the future appears a lot less bleak than it did at this point one year ago. But there remains a great deal of unrest and uncertainty. What does it mean for job searchers in the 2021–2022 market? The key to a successful job search will be flexibility. Open your minds, your requirements, and your maps. The market is still depressed, and the best jobs will fill quickly. Savvy employers will look for candidates selecting jobs for the long term and for the right reasons. There will be concern among many employers that graduating residents are using those jobs as stepping stones until becoming ABEM-certified, so they then risk losing that talent to another employer. New graduates may need to dial back a bit on their location and lifestyle demands and focus more on choosing real opportunities that will be the building blocks of a successful career in emergency medicine. Plus-circle
Reference
- Hartnett KP, Kite-Powell A, DeVies J, et al. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699-704.
Ms. Katz is president of The Katz Company EMC, a member of ACEP’s Workforce and Career sections, and a frequent speaker and faculty at conferences and residency programs. She can be reached at katzco@cox.net.
Pages: 1 2 3 | Multi-Page





2 Responses to “2021 Survey of the Emergency Medicine Job Market”
October 24, 2021
Steven M Winograd MD FACEPYour survey was most important. I see in the New York City area, many midlevels replacing Attendings, so that Attendings are supervising a larger number of midlevels. After 2 midlevels it becomes undoable, so actually “some” midlevels are really not being supervised at all. At Urgent Cares, most midlevels are really not being supervised. Since the salary of an Attending is equivalent to 3 midlevels, it “is” all about saving money.
November 13, 2021
Dr.Danvanilla Quansha BarbesI’m doctor Danvanilla Barnes I’m new license doctor in Clewiston Florida..
Something I have never experienced yet..But I’m learning to be a better doctor.And improving my skills to be a successful woman black leader in medical field ..I pray you welcome me with open arms and a big
Stay safe COVID 19
Wash hands wear mask and be germ free
Dr.Danvanilla Q Barnes