A 20-year-old healthy man arrives at the emergency department at 4 a.m. complaining of one hour of excruciating right testicular pain that radiates to his right lower quadrant and right flank. He’s been vomiting repeatedly. He has had no preceding lower urinary tract symptoms. Vitals are normal except for a heart rate of 115. His right testicle appears swollen with a horizontal high-riding lie and is exquisitely tender to palpation. The cremasteric reflex is absent on the right side.
Explore This Issue
ACEP Now: Vol 39 – No 10 – October 2020This is a relatively straightforward case for the diagnosis of testicular torsion, but unfortunately most cases of testicular torsion are not so clear-cut; the classic symptoms and signs often are not present. That is why 30 percent of the cases with failed testicular salvage can be attributed to misdiagnosis, with another 13 percent to delays in treatment after the diagnosis has been made.1
1. Time counts, but salvageability is possible more than 48 hours after symptom onset.
Testicular torsion is a surgical emergency regardless of the time of onset. The spermatic cord twists, leading to impaired blood flow to the testicle, which causes ischemia and tissue necrosis. The degree of twisting and duration of symptoms are prognostic factors of testis salvage, with 96 percent success rates when perfusion is restored within four hours. Salvage is less than 10 percent if interventions are delayed for more than 24 hours.2,3 Nonetheless, salvageability has been shown beyond 48 hours after symptom onset, contrary to the historical teaching that symptoms of more than 24 hours are inconsistent with salvageable tissue. In delayed cases that are salvageable, there may be intermittent, rather than continuous, twisting of the spermatic cord, allowing reperfusion of the testicle. Therefore, it is incumbent on emergency physicians to manage all acute scrotum cases as surgical emergencies, even if the time from onset to presentation exceeds 24 hours.
2. Testicular torsion can occur at any age.
Testicular torsion has a bimodal distribution: first year of life and in adolescence. I’ve had urologists tell me emphatically that testicular torsion does not occur in patients older than 40 years of age. Nonetheless, in a study of 469 closed malpractice claims with indemnity payment, the mean age was 23 years and there were four patients over the age of 40.4 The literature is rife with case reports of older patients with surgically confirmed testicular torsion.5–8
3. Testicular torsion can present with minimal, intermittent, or no scrotal pain.
While a sudden onset of severe, unrelenting unilateral scrotal pain radiating to the abdomen and/or flank is typical, the pain of testicular torsion can also be minimal or intermittent—again, attributed to intermittent twisting and untwisting of the spermatic cord that occurs in some cases.9 These “pain honeymoons” may partially account for poor clinical outcomes. As many as 20 percent of patients with testicular torsion present with isolated lower abdominal pain.10 In light of this, all male patients presenting with lower abdominal pain should have a genital examination for signs of torsion.
4. There is no single symptom or sign or combination of clinical features that has adequate predictive value in ruling out testicular torsion.11
Of particular importance is that the presence of a cremasteric reflex does not rule out the diagnosis. Studies report varying sensitivities as low as 60 percent and odds ratios (ORs) from 4.8 to 27.8.12,13 While the presence of an elevated testicle (OR=58.8) and a horizontal testicular lie increase the likelihood of testicular torsion, it is often difficult to palpate the testicle only, thereby determining its position relative to other adjacent structures.14 Scrotal erythema, edema, and testicular swelling are commonly reported in patients with torsion. However, these findings are also commonly found in patients with epididymitis and torsion of the appendix testis.13 Prehn’s sign is the relief of pain with elevation of the testicle, historically thought to be common in patients with epididymitis. This physical examination finding does not reliably distinguish epididymitis from torsion. One cross-sectional study of 120 patients found the Prehn’s sign was present in 91 percent of patients with torsion and 21 percent of those with epididymitis.15
In 2013, an attempt at combining clinical features of testicular torsion in a clinical decision tool for the diagnosis of testicular torsion yielded the TWIST (Testicular Workup for Ischemia and Suspected Torsion) score. While this score showed a 100 percent positive predictive value when all clinical findings were present, potentially obviating the need for Doppler ultrasound imaging confirmation of the diagnosis, it failed to show adequate negative predictive value in ruling out the diagnosis clinically.16 Hence, all patients with any suspicion for testicular torsion should have urgent Doppler ultrasound imaging and/or urological consultation.
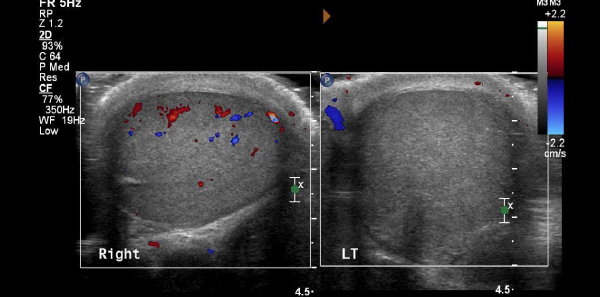
5. Doppler ultrasound has significant limitations in the diagnosis of testicular torsion.
If clinical features cannot rule out torsion, can a Doppler ultrasound? Typically, Doppler ultrasound findings for testicular torsion include an enlarged, hyperemic testicle; decreased Doppler flow to the parenchyma of the testicle itself; and a “whirlpool sign” (a spiral-like pattern of the spermatic cord twisting).17,18 Unfortunately, the test characteristics of Doppler ultrasound are far from perfect, and it is subject to false negatives; the spermatic cord may untwist while the ultrasound is being performed and re-twist afterwards. Alternatively, a partially-torsed testicle may exhibit arterial flow but no venous flow, or it may show an abnormal high-resistance pattern of arterial flow. The sensitivity of Doppler ultrasound ranges from 88 to 100 percent.17 When ultrasound is nondiagnostic and the clinical presentation remains concerning, urology consultation remains warranted. The gold standard for diagnosis and exclusion of testicular torsion is surgical exploration.
Conclusion
Next time you are faced with a patient with acute lower abdominal and/or scrotal pain, consider the diagnosis of testicular torsion regardless of age. Understand that the duration of symptoms should not guide urgency of management and that all cases of suspected testicular torsion must be treated as a surgical emergency. Remember that the presence of a cremasteric reflex does not rule out testicular torsion and that all clinical characteristics and even Doppler ultrasound have significant limitations in making or excluding the diagnosis. Urological consultation should always be obtained in equivocal cases.
Special thanks to Dr. Natalie Wolpert and Dr. Yonah Krakowsky for their expert contributions to the EM Cases podcast that inspired this article.
References
- Davis JE, Silverman M. Scrotal emergencies. Emerg Med Clin North Am. 2011;29(3):469-484.
- Howe AS, Vasudevan V, Kongnyuy M, et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol. 2017;6(6):1159-1166.
- Mellick LB, Sinex JE, Gibson RW, et al. A systematic review of testicle survival time after a torsion event. Pediatr Emerg Care. 2019;35(12):821-825.
- Perrotti M, Badger W, Prader S, et al. Medical malpractice in urology, 1985 to 2004: 469 consecutive cases closed with indemnity payment. J Urol. 2006;176(5):2154-2157.
- Mejdoub I, Fourati M, Rekik S, et al. Testicular torsion in older men: it must always be considered. Urol Case Rep. 2018;21:1-2.
- Tang YH, Yeung VHW, Chu PSK, et al. A 55-year-old man with right testicular pain: too old for torsion? Urol Case Rep. 2017;11:74-75.
- Farrington NL, Lucky MA, Barnes T, et al. Confirmed testicular torsion in a 67 year old. J Surg Case Rep. 2014;2014(1):rjt119.
- Alqasem S, Alhamdan A, Alhefzi A, et al. Acute scrotum in elderly; is it torsion! Urol Case Rep. 2020;28:101032.
- Mellick LB, Sinex J. Testicular torsion pain honeymoons. Pediatr Emerg Care. 2019;35(12):e241-e244.
- Wang F, Mo Z. Clinical evaluation of testicular torsion presenting with acute abdominal pain in young males. Asian J Urol. 2019;6(4):368-372.
- Ciftci AO, Senocak ME, Tanyel FC, et al. Clinical predictors for differential diagnosis of acute scrotum. Eur J Pediatr Surg. 2004;14(5):333-338.
- Mellick LB. Torsion of the testicle: it is time to stop tossing the dice. Pediatr Emerg Care. 2012;28(1):80-86.
- Paul EM, Alvayay C, Palmer LS. How useful is the cremasteric reflex in diagnosing testicular torsion? [Supplement]. J Am Coll Surg. 2004;199(3):101.
- Beni-Israel T, Goldman M, Bar Chaim S, et al. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med. 2010; 28(7):786-789.
- Roth B, Giannakis I, Ricklin ME, et al. An accurate diagnostic pathway helps to correctly distinguish between the possible causes of acute scrotum. Oman Med J. 2018;33(1):55-60.
- Frohlich LC, Paydar-Darian N, Cilento Jr BG, et al. Prospective validation of clinical score for males presenting with an acute scrotum. Acad Emerg Med. 2017;24(12):1474-1482.
- Bandarkar AN, Blask AR. Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis. Pediatr Radiol. 2018;48(5):735-744.
- McDowall J, Adam A, Gerber L, et al. The ultrasonographic “whirlpool sign” in testicular torsion: valuable tool or waste of valuable time? A systematic review and meta-analysis. Emerg Radiol. 2018;25(3):281-292.
Pages: 1 2 3 4 | Multi-Page



No Responses to “5 Tips on Testicular Torsion”