You may already know the names: vancomycin-resistant Staphylococcus aureus (VRSA), carbapenem-resistant Pseudomonas aeruginosa (CRPA), extended-spectrum beta-lactamase (ESBL) Escherichia coli. These are just some of the next-generation “superbugs” that are popping up in emergency departments across the United States. In 2018, 12 of the most concerning multidrug-resistant organisms (MDROs) were ranked by lethality, earning the nickname “the dirty dozen.”1 More concerning is that some of these bacteria, like the carbapenem-resistant Klebsiella pneumoniae that recently resulted in fatal sepsis for a woman in Reno, Nevada, are resistant to all available antibiotics. In other words, they are invincible.2
Explore This Issue
ACEP Now: Vol 39 – No 02 – February 2020Or are they? The antibiotic pipeline has largely dried up in recent years, so what can emergency physicians do to combat MDROs?3 Antibiotic stewardship.4 As Benjamin Franklin said, “An ounce of prevention is worth a pound of cure.”
When we unnecessarily prescribe antibiotics for viruses, misdiagnose noninfectious conditions (eg, pseudocellulitis), or provide suboptimal antibiotic regimens, we exert selective pressure on our local community’s biome. Selective pressure encourages resistant bacteria to thrive by killing off weaker bacteria.
It is not too late. We are living in a crucial time. The prevalence of superbugs remains low in most communities. By practicing what we call the “5 D’s of antibiotic stewardship”—right diagnosis, right drug, right dose, right duration, right de-escalation—we can reduce the prevalence of MDROs in our hospitals and communities.5 Future generations will thank us—or better yet, they won’t even realize they have to.
Meet the 5 D’s
Here are the 5 D’s applied to emergency medicine practice.
- Right Diagnosis: Take a diagnostic stand and call a virus a virus. Acute otitis media, bronchitis, sinusitis—all of these entities are far more often viral than bacterial. When the patient is not seriously ill, is not immunocompromised, and clearly had a recent viral prodrome, you can usually avoid antibiotics.
- Right Drug: For patients with uncomplicated bacterial infections that require antibiotics, consult your institution’s ED antibiogram to identify the most common causative organism and narrowest spectrum agent that is typically effective (eg, nitrofurantoin for Escherichia coli).
- Right Dose: Practice weight-based dosing of antibiotics for pediatric patients, and for noncritically ill adults, err on the low side of the suggested dose range.
- Right Duration: It is a poorly-kept secret in medicine that the recommended length of most antibiotic regimens was chosen arbitrarily in initial studies and has been subject to inertia ever since. When offered a range of duration of therapy, choose the shortest duration. If you are prescribing any antibiotic for more than seven days, favor a shorter course.6–9
- Right De-escalation: Antibiotic de-escalation is a new trend in emergency medicine. Emergency physicians make decisions that generate therapeutic momentum for inpatient antibiotic prescribing. The act of simply writing in the chart, “These broad-spectrum agents should be narrowed to a single-effective agent once culture results have returned,” can save your patients days of unnecessary antibiotics.
For those looking for more specific ways to implement the 5 D’s, we have provided our five tips you can use on your next shift (see Table 1).
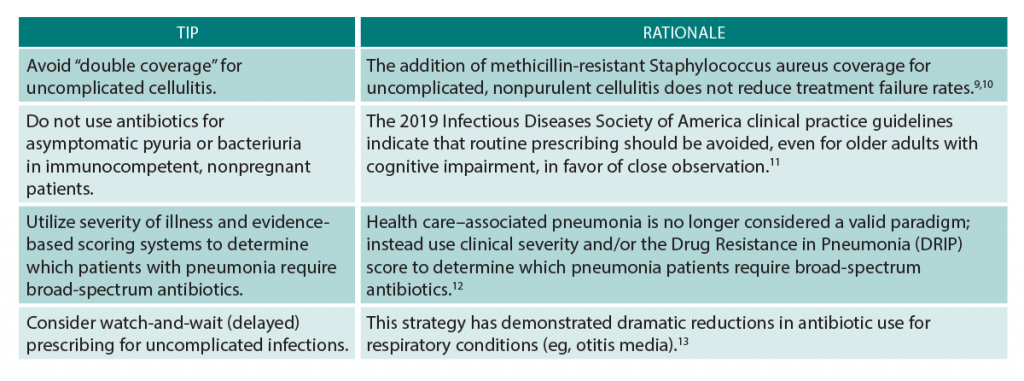
(click for larger image) Table 1: Top 5 Tips to Improve Antibiotic Stewardship in the Emergency Department
Become a Champion for Your ED
Ready for the next level? What about becoming an ED antibiotic stewardship champion or starting an ED-specific antibiotic stewardship program? Yes, this is in our wheelhouse!
Hospital antibiotic stewardship programs are now required by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS), and emergency medicine needs to have a seat at the germ-infested table. Practicing at the intersection of the community and the hospital, we are the frontline providers for patients with MDROs. Our role is to try to select the correct initial antibiotic, despite diagnostic uncertainty. This unique and often challenging task requires an informed plan. We, as emergency physicians, should be the ones making the plan, not just following orders from others who don’t have experience doing what we actually do.
For an in-depth implementation guide to antibiotic stewardship in the emergency department, check out the MITIGATE toolkit. This tool takes the Centers for Disease Control and Prevention’s recommended core elements for outpatient antibiotic stewardship (which include a commitment to using antibiotics appropriately, implementing one policy or practice, tracking and reporting, education, and expertise) and adapts them to emergency department and urgent care settings. The toolkit leverages improvement science and behavioral economics to nudge clinicians to do the right thing in avoiding antibiotics for viral infections.
ED champions are critical to any program’s success. Interventions are more effective when they take the unique ED environment and workflow into account.
Still on the fence about leading the antibiotic stewardship charge? There are plenty of other ways you can start to engage beyond day-to-day patient care.
First, make sure someone from your emergency department sits on the antibiotic stewardship committee. Think about how local guidelines and clinical pathways can support better antibiotic use. For instance, do you really need a urine sample in the nurse-driven order set for chest pain? How about working with pharmacy and therapeutics to develop an empiric antibiotic prescribing guide based on antibiograms for your emergency department? The same goes for sepsis order sets, which should include evidence-based empiric antibiotic prescribing decision support. We can even facilitate de-escalation by making sure relevant cultures are ordered.
The goal of antibiotic stewardship programs is to improve patient outcomes, but they can also make your life easier. Find out the pain points to optimizing antibiotic use in your emergency department and then design a simple quality improvement project to fix them. There are a number of stewardship targets to explore, and some of these efforts can be made seamless through the use of behavioral nudging—for example, setting a default duration for antibiotics in your electronic health record by indication or making the first-line agents pop up for the default diagnosis. These fixes are better for patient care, they preserve physician autonomy, and they require fewer clicks. Win-win-win.
The fight against superbugs and MDROs is not coming to our emergency department’s doorstep; it is already here. As the frontline physicians for any epidemic, we will be the ones wearing the hazmat suits, placing the central line to hang the fourth antibiotic, and watching our patients suffer. ACEP has a team of emergency physicians working to prepare antibiotic stewardship resources for our workforce. In the meantime, we ask, Are you ready to step up and be an antibiotic steward? Is your emergency department ready for an antibiotic stewardship program? And before we just throw broad-spectrum agents into an IV, what the heck is the source of that 102°F fever in the patient in bed four?
Dr. Redwood is an emergency and preventive medicine physician and associate medical director of emergency medicine at Cooley Dickinson Hospital in Northampton, Massachusetts.
Dr. May is professor of emergency medicine and director of emergency department antibiotic and outpatient stewardship at UC Davis Health in Sacramento.
Dr. Pulia is director of the emergency department antibiotic stewardship program at the BerbeeWalsh Department of Emergency Medicine at University of Wisconsin, Madison.
References
- Shrivastava SR, Shrivastava PS, Ramasamy J. World Health Organization releases global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics. J Med Soc. 2018;32(1):76-77.
- Ofori-Asenso R. “When the bug cannot be killed”—the rising challenge of antimicrobial resistance. Medicines (Basel). 2017;4(2): pii:E40.
- Livermore DM, British Society for Antimicrobial Chemotherapy Working Party on The Urgent Need: Regenerating Antibacterial Drug Discovery and Development. Discovery research: the scientific challenge of finding new antibiotics. J Antimicrob Chemother. 2011;66(9):1941-1944.
- May L, Cosgrove S, L’Archeveque M, et al. A call to action for antimicrobial stewardship in the emergency department: approaches and strategies. Ann Emerg Med. 2013;62(1):69-77.
- Pulia M, Redwood R, May L. Antimicrobial stewardship in the emergency department. Emerg Med Clin North Am. 2018;36(4):853-872.
- Dawson-Hahn EE, Mickan S, Onakpoya I, et al. Short-course versus long-course oral antibiotic treatment for infections treated in outpatient settings: a review of systematic reviews. Fam Pract. 2017;34(5):511-519.
- Havey TC, Fowler RA, Daneman N. Duration of antibiotic therapy for bacteremia: a systematic review and meta-analysis. Crit Care. 2011;15(6):R267.
- Michael M, Hodson EM, Craig JC, et al. Short compared with standard duration of antibiotic treatment for urinary tract infection: a systematic review of randomised controlled trials. Arch Dis Child. 2002;87(2):118-123.
- Moran GJ, Krishnadasan A, Mower WR, et al. Effect of cephalexin plus trimethoprim-sulfamethoxazole vs cephalexin alone on clinical cure of uncomplicated cellulitis: a randomized clinical trial. JAMA. 2017;317(20):2088-2096.
- Pallin DJ, Binder WD, Allen MB, et al. Clinical trial: comparative effectiveness of cephalexin plus trimethoprim-sulfamethoxazole versus cephalexin alone for treatment of uncomplicated cellulitis: a randomized controlled trial. Clin Infect Dis. 2013;56(12):1754-1762.
- Nicolle LE, Gupta K, Bradley SF, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis. 2019;68(10):e83-e110.
- Webb BJ, Sorensen J, Mecham I, et al. Antibiotic use and outcomes after implementation of the drug resistance in pneumonia score in ED patients with community-onset pneumonia. Chest. 2019;156(5):843-851.
- Spurling GK, Del Mar CB, Dooley L, et al. Delayed antibiotic prescriptions for respiratory infections. Cochrane Database Syst Rev. 2017;9:CD004417.
- Davis LC, Covey RB, Weston JS, et al. Pharmacist-driven antimicrobial optimization in the emergency department. Am J Health Syst Pharm. 2016;73(5 Suppl 1):S49-56.
- Randolph TC, Parker A, Meyer L, et al. Effect of a pharmacist-managed culture review process on antimicrobial therapy in an emergency department. Am J Health Syst Pharm. 2011;68(10):916-919.
Pages: 1 2 3 4 | Multi-Page





No Responses to “5 Tips to Improve Antibiotic Stewardship in Your Emergency Department”