A simpler modified method involves using the pulse oximeter before and after the patient receives 100 percent oxygen (or as close to a 100 percent FiO2 as possible) for five to 10 minutes and noting whether the oxygen saturation improves. If the oxygen saturation improves, the underlying cause of the oxygen desaturation favors a respiratory etiology. But if the oxygen saturation does not improve, a cardiac cause is more likely.
Explore This Issue
ACEP Now: Vol 37 – No 05 – May 2018Proceed with caution when administering the hyperoxia test. Oxygen is a potent pulmonary vasodilator and could worsen respiratory distress in a patient with a duct-dependent lesion by decreasing pulmonary vascular resistance (PVR) and increasing pulmonary blood flow, leading to pulmonary over-circulation.
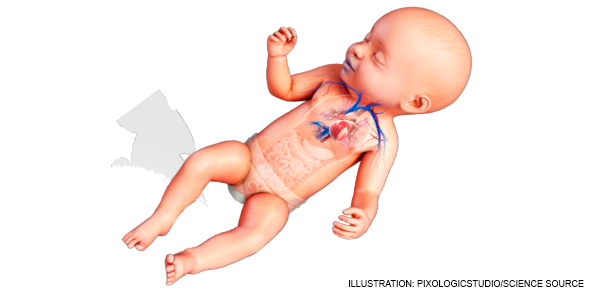
There are three physical exam maneuvers to consider involving limb-pulse differentials: 1) a pulse delay between radial (preductal) and femoral (postductal) pulses (or absence of femoral pulses); 2) a blood pressure differential between the right upper and a lower extremity; and 3) a difference in pulse oximetry of more than 3 percent between the right upper and a lower extremity. These all suggest a duct-dependent lesion.4
Pediatric ECG interpretation can prove challenging for many community physicians. A simple approach with regard to CHD involves the presence or absence of ventricular hypertrophy. The ECG can suggest CHD if there is evidence of LVH at any age or RVH after 1 month of age.5,6 It’s important to note that normal newborns exhibit high right-side pressures with right axis deviation and signs of RVH on the ECG. However, persistent high right-side pressures and RVH after 1 month of age is likely due to a cardiac obstructive lesion.
If you have acquired advanced cardiac ultrasound skills, bedside ultrasound may offer some clues to the underlying diagnosis in an acutely ill CHD patient.7 Ask yourself three simple questions:
- Is the global cardiac function poor (a sign of heart failure)?
- Are there four chambers of the heart (some congenital cardiac lesions involve the absence of one or more cardiac chambers)?
- Is the septum intact (consider VSD and PDA)?
Treatment Considerations
When presented with gray or blue infants suspected of duct-dependent lesions in your emergency department, CHD should be in your differential diagnosis, but it is important to remember sepsis is far more common, and as such, early empiric antibiotics should be started as soon as possible. Start prostaglandin therapy for all acutely ill gray or blue infants younger than 1 month of age to keep the PDA open. Be prepared to intubate and resuscitate the neonate who receives prostaglandins because prostaglandins can cause apnea as well as severe hypotension.
Pages: 1 2 3 4 | Single Page





4 Responses to “A 3-Step Approach for Infants with Congenital Heart Disease”
June 7, 2018
Hexham khaledExcellent
February 25, 2019
Iman Ali Ba-SaddikA simplified approach which serves as a very good practical guide to congenital heart disease
July 5, 2019
Sunita Harkar ShallaWell written and very informative.
July 22, 2020
AmeenVery informative, Thank you so much.