Lancaster General Hospital (LGH), in Lancaster, Pa., has long had a reputation for an efficient, busy, community hospital emergency department (ED). Now part of Penn Medicine Health System, it is a 525-bed, nonprofit, level I trauma center, and offers both Percutaneous Coronary Intervention (PCI) and stroke thrombectomy. It has American Nurses Credentialing Center magnet designation. Its ED sees 113,000 visits a year and a high volume of geriatric patients (28.5 percent). Prior to 2021, the ED boasted some of the best operational metrics reported in an ED of its size and could be considered a “best of breed.” Its door-to-doctor time was 25 minutes and its walkaway rate only 1.7 percent. After COVID-19, however, with increasing behavioral health (BH) volumes and increasing boarding, the department began to falter. In 2021 those metrics were 40 minutes and 9.2 percent, respectively.
Explore This Issue
ACEP Now: Vol 42 – No 05 – May 2023While the community presented with as many BH complaints as chest pain chief complaints, there was no comprehensive service line dedicated to mental health issues. In addition, the community resources for such patients were limited. Historically, the ED had operated under a traditional flow model, beginning with nurse triage, and with further health care interactions operating in series in the main department. They had not begun a flow model involving a physician in triage (PIT), which is now considered a best practice for high-volume EDs.
Thinking Differently
LGH decided that their current structure was not functioning and that a new flow model was required, particularly for the BH patients. Because they had a vast waiting room with more than 70 plexiglass-enclosed chairs, but treatment spaces with beds were limited in the main part of the ED, LGH began thinking about ways to use existing resources differently.
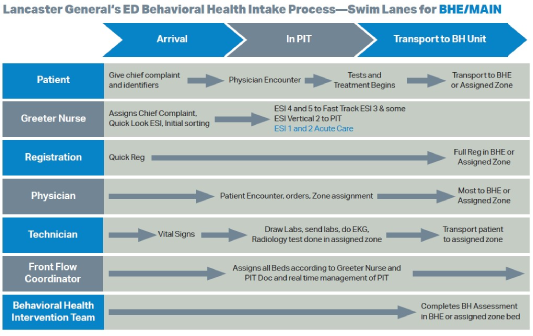
A task force set out to manage BH patients differently. The ED clinical team—in conjunction with the dedicated BH team—worked collaboratively together to determine best flow for patients arriving with a BH complaint. When the PIT doc is present, patients are seen and assessed in tandem by a triage nurse and a physician. The PIT team can initiate a BH consult while the patient remains in triage; when possible, patients are discharged directly from the triage area after the medical screening exam and the BH team assessment (backed by a psychiatrist). This has resulted in a reduction in one-to-one sitter usage for discharged patients, and expedites bed search for patients requiring psychiatric admission.
The swim lane diagram (see Figure 1) shows the process they developed.
Meanwhile, the LGH Hospital leadership team re-conceptualized the BH space altogether. Rather than serving as a holding area for acutely psychotic or suicidal patients waiting for placement, they created a small unit that follows the psychiatric assessment, treatment and healing (PATH) model. Figure 2 shows the newly conceptualized PATH model.
Some of the features of this unit include:
- Ligature-free rooms and common hallway spaces
- Lockers to store patient belongings safely and privately
- Medication-reconciliation specialist in ED
- Security stationed in unit
- Duress buttons provided for every staff member
- Care team: ED registered nurse, BH intervention team (BHIT) member, psychiatry consults when applicable
- Laundry area in unit, overflow rooms with garage doors
The LGH ED overall and within the PATH unit has another innovative process to mitigate elopements. The Rauland call-bell system in the unit is enabled when the yellow E button is depressed.
When activated the PATH area becomes a locked unit. Patients who pose suicide or elopement risk wear bright yellow gowns for easy identification. The yellow E technology has proven to reduce and prevent patient elopements.
PIT has improved overall median length of stay (LOS) and earlier BH assessment. The data show that BH patients managed through the BHIT process in triage consistently have shorter LOS than BH patients managed using a traditional flow model.
The LGH leadership team invented a model for BH patients using available resources that could be replicated elsewhere. The Lancaster General Hospital ED is proud of its success in managing their BH burden; Bit by BHIT they know they have found the right PATH to do so!
 Dr. Welch was a practicing emergency physician for more than 30 years and a research fellow at the Intermountain Institute for Health Care Delivery Research in Murray, Utah. She has written numerous articles and three books on ED quality, safety, and efficiency. She is a consultant with Quality Matters Consulting, and her expertise is in ED operations.
Dr. Welch was a practicing emergency physician for more than 30 years and a research fellow at the Intermountain Institute for Health Care Delivery Research in Murray, Utah. She has written numerous articles and three books on ED quality, safety, and efficiency. She is a consultant with Quality Matters Consulting, and her expertise is in ED operations.
Pages: 1 2 | Multi-Page





No Responses to “A Behavioral Health Intake-Process Model”