This decontextualized response is also challenging for responders. In one ED in the San Francisco area, a law enforcement officer staffed there said they would appreciate additional support for de-escalating patients. From the law enforcement perspective, hospital policies regarding behavioral codes were “vague” and the same patients are often seen multiple times with similar behavioral crises, he noted in an interview. Both security and health care teams assisting during these crises may benefit from a re-framing of the response to mentally vulnerable patients during times of aggression.
Explore This Issue
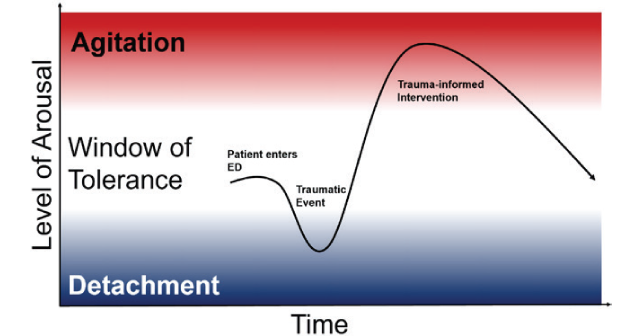
ACEP Now: Vol 42 – No 11 – November 2023When a patient first enters the ED, they may be within their window of tolerance of stimuli and interventions, (see Figure 2) but a triggering event may cause an initial detached state (numb, quiet, dissociated) to a hyper-aroused agitated state (yelling, getting out of bed, throwing objects). Trauma-informed interventions deployed by BERTs use de-escalation techniques to move the patient from the hyper-aroused state back into the window of tolerance so that they can effectively engage in their care.
A Call for Change: BERTs
Just as rapid response teams have been created to attend urgently to medically decompensating patients in the hospital, Behavioral Emergency Response Teams (BERTs) have been created to rapidly identify and tend to a patient whose behavior is escalating. Evidence from inpatient wards, outpatient facilities, and addiction treatment centers has demonstrated that BERTs are an effective de-escalation solution in a variety of care contexts.
A 2019 literature review summarized seven studies describing the creation and implementation of BERT teams. Led by psychiatric-trained nurses, teams responding to behavioral codes used a variety of de-escalation methods including non-confrontational communication, moving the patient to a less stimulating environment, and adjusting medications as necessary. Across clinical contexts, BERT teams reduced the activity of security personnel, restraint and seclusion use, and staff injuries.5 A University of Kansas study found that their BERT structure fosters “a collaborative team within the ED and provides a model of humane care.”4
Conclusion
More implementation studies of this emerging behavioral solution in resource-limited emergency settings are needed. Our group from Highland Hospital has set out to understand the impact on workplace violence and patient safety of initiating a BERT in a busy, county hospital ED. “The workplace violence data in emergency departments are staggering, and it can feel defeating, especially when we and our colleagues experience it firsthand,” explains Dr. Nikita Joshi, faculty lead for efforts to reduce workplace violence in the county health system. “But BERT is an important initiative to proactively address it–in a way that is patient centric, trauma informed, and most of all, empathic toward the patient and the clinician.” The well-being of our patients, staff, and ourselves depends on finding tailored and effective solutions and dissemination of these best practices.
Pages: 1 2 3 | Single Page




No Responses to “A Safety Solution for Emergency Department Staff and Patients”