The accreditation criteria for each tier are summarized in Table 2. Level 3 GEDs represent expectations attainable by smaller hospitals, often in rural settings in which around-the-clock access to advanced imaging or labs may be limited and where staffing often includes non-physician providers. The level 3 criteria reflect these more limited resources. The level 2 criteria add expectations for demonstrable geriatric-focused staff education and guidelines as well as regular outcomes linked to specific process changes. Level 2 GEDs would be expected to achieve 75 percent adherence to at least 10 (out of 26) best practices on random chart audits of 10 total patients occurring quarterly, and they should be able to report on at least 25 percent of relevant outcome measures. Level 1 GEDs would serve as the gold standard of geriatric emergency care, demonstrating excellence by fulfilling the same criteria as Level 2 but with the addition of patient stakeholder representation, dedicated space or structures, and reporting of at least 50 percent of relevant outcome measures.
Explore This Issue
ACEP Now: Vol 36 – No 04 – April 2017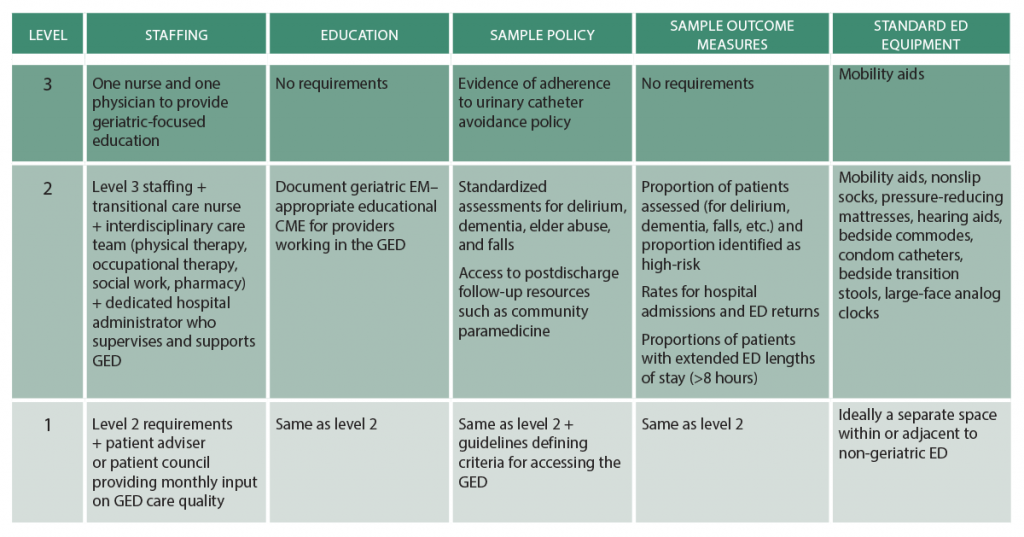
(click for larger image) Table 2: Comparisons of Established Definitions, Sepsis-3 Definitions, and SSC Guidelines
The ACEP GEDA taskforce and Board of Directors are well aware of the ever-increasing and largely unreimbursed quality and educational requirements placed on ACEP members. Being mindful of this, accreditation relies on self-reporting, has minimal associated cost, and incurs no additional CME requirements. We anticipate the accreditation process, and subsequent recognition of GED hospitals, will create a standardized and quantifiable program aligning the GED guidelines and GED accreditation with hospitals’ priorities. ACEP members at GED-accredited hospitals should therefore benefit from greater hospital resources and support that better address the needs of geriatric patients, providers, and health care systems, which ultimately will improve the care delivered to geriatric ED patients. As observed in other areas of emergency medicine, non–emergency medicine organizations could potentially dictate GED accreditation with little knowledge of the issues important to emergency physicians. Emergency physicians are setting the standard, and thus, ACEP is seizing the opportunity to determine and define our own best practices and to support the delivery of emergency care for its members.
Dr. Carpenter is associate professor of emergency medicine and director of evidence based medicine at Washington University School of Medicine in St. Louis. Dr. Hwang is associate professor in the departments of emergency medicine and the Brookdale Department of Geriatrics and Palliative Medicine Icahn School of Medicine at Mount Sinai in New York City and research faculty at the Geriatric Research, Education, and Clinical Center at the James J. Peters VAMC in Bronx, New York. Dr. Biese is associate professor of emergency medicine and internal medicine, division of geriatrics, at the University of North Carolina at Chapel Hill School of Medicine. is program director of the Comprehensive Advanced Life Support Program in Minneapolis. Dr. Hogan is associate professor, sections of emergency medicine and geriatric and palliative medicine, at the University of Chicago. Dr. Karounos is chief of the geriatric emergency department and director of research at St. Joseph’s Healthcare System in Paterson, New Jersey. Dr. Malone is the medical director of senior services at Aurora Health Care and serves as the American Geriatrics Society’s liaison to ACEP. Dr. Melady is an emergency physician at the Schwartz/Reisman Emergency Medicine Institute at Mount Sinai Hospital in Toronto. Dr. Rosen is assistant attending physician at NewYork-Presbyterian Hospital in New York City. Dr. Rosenberg is chairman of emergency medicine and associate professor of clinical emergency medicine at St. Joseph’s Healthcare System. Dr. Schneider is director of EM practice at ACEP. Dr. Shah is associate professor and vice chair for research and academic affairs in the department of emergency medicine at the University of Wisconsin School of Medicine and Public Health in Madison. Dr. Spiegel is assistant professor of medicine and medical director for the Mitchell Emergency Department at the University of Chicago Department of Medicine. Dr. Stern is assistant professor of medicine in emergency medicine and chief of geriatric emergency medicine at NewYork-Presbyterian Hospital/Weill Cornell Medical Center in New York City.
References
- Hwang U, Shah MN, Han JH, et al. Transforming emergency care for older adults. Health Aff (Millwodd). 2013;32(12):2116-2121.
- Rosenberg MS, Carpenter CR, Bromley M, et al. Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7-e25.
- Hogan TM, Olade TO, Carpenter CR. A profile of acute care in an aging America: snowball sample identification and characterization of United States geriatric emergency departments in 2013. Acad Emerg Med. 2014;21(3):337-346.
Pages: 1 2 3 | Single Page





No Responses to “ACEP Accredits Geriatric Emergency Care for Emergency Departments”