ACEP endorsed the latest iteration of the Surviving Sepsis Campaign (SSC) guidelines, totaling 67 pages with 93 statements on early management and 655 references.1,2 An important note: Guidelines should be a counselor, not a jailer. Guidelines provide a framework for direction and standardization where possible but require clinical context for individual patients. This summary includes items specifically pertinent to emergency medicine and is not intended to be all-inclusive.
Explore This Issue
ACEP Now: Vol 36 – No 03 – March 2017Definitions
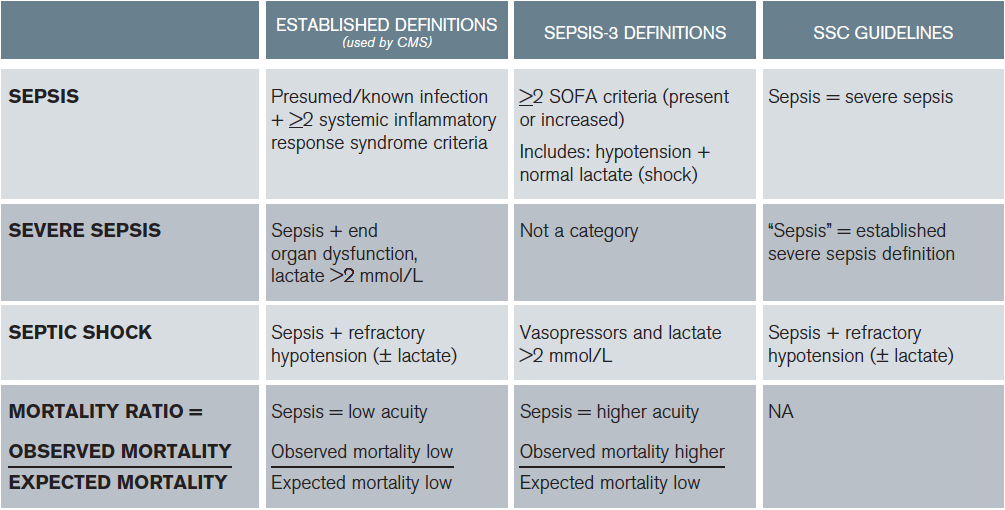
All the data informing guideline development were based on the established definitions, not Sepsis-3. The Sepsis-3 and established definitions were modified for the purpose of guideline application.3 In the 2016 SSC guidelines, sepsis equates to the established definitions of severe sepsis (infection + organ dysfunction, including hyperlactemia) and septic shock (hypotension ± lactate). The Quick Sepsis Related Organ Failure Assessment (qSOFA) did not inform any part of the guidelines. ACEP and other organizations did not support or endorse the Sepsis-3 definitions due to patient safety concerns.4,5 The SSC guidelines acknowledged that:
- There is insufficient data to apply the Sepsis-3 definitions to the guidelines.
- Lactate is important and part of the established definition of severe sepsis (or sepsis in the guidelines). Additionally, the guidelines highlight the importance of lactate normalization. Both early monitoring and early management of hyperlactemia are key components of emergent resuscitation and patient care principles important in ACEP’s decision to support the guidelines when it did not support the Sepsis-3 definitions.
Consistent with the law of unintended consequences, even when compatible care is provided, clinicians implementing Sepsis-3 definitions may appear to provide worse care than those using established definitions on national quality metrics (see Table 1). So now there are three definitions: the established definitions, the SSC definitions that are based on the established definitions, and the Sepsis-3 definitions (see Table 1). What a mess. Which ones do we use? I suggest that we use the established definitions for care.
(click for larger image)
Table 1: Comparisons of Established Definitions, Sepsis-3 Definitions, and SSC Guidelines
Mortality ratio, national quality metrics based on established definitions (expected mortality). When clinicians apply a low-acuity diagnosis (sepsis) to a higher-acuity patient (Sepsis-3 definition of sepsis), the observed mortality will be higher than expected. Results in similar care appearing worse based on different definitions applied to the same patients. Note: CMS recognizes normotension + lactate ≥ 4 as septic shock
Perhaps future prospective evaluation will support the use of Sepsis-3 and qSOFA. However, that should be played out in further academic work and not via national payment metrics.
Pages: 1 2 3 4 5 | Single Page




5 Responses to “ACEP Endorses Latest Surviving Sepsis Campaign Recommendations”
March 31, 2017
John ReevesWell done review! Thank you so much – very helpful
April 2, 2017
Munish GoyalGreat work, Tiffany. This very nicely summarizes the different definitions, some of the confusion, and a logical path forward.
One thing caught my eye in table 1 — the established definition (CMS) of severe sepsis includes an elevated lactate (> 2.1 at my shop), not lactate > 4.
April 28, 2017
Dawn Antoline-WangThank you for pointing this out, Dr. Goyal. The table has been corrected.
March 18, 2018
Rushdi AlulHello Dr. Osborn,
I am an internist working in the Chicago area and I would like to commend you for writing such an excellent article. I am contacting you in regard to a comment in your article, specifically your recommendation to use the established definitions for sepsis used by CMS. My confusion is the following. I will see on a regular basis young adults, for example, a 21 year old male complaining of fever and sore throat and noted to have a heart rate >90 bpm. After examination if appropriate, I will perform a rapid strep test. Assuming the strep test is positive I will tell him he has strep throat and treat him accordingly. However he meets the CMS guideline for sepsis, is his correct diagnosis strep throat with sepsis?? I am reluctant to use sepsis in this scenario since I am accustomed to associating sepsis with patients who display evidence of clinical or hemodynamic instability (requiring resuscitative intervention) which this young man does not have nor need. Any clarification or insight you can provide would be greatly appreciated!
March 20, 2018
Rushdi AlulDr. Osborn,
I would like to commend you for writing such an excellent article. I am contacting you in regard to a comment in your article, specifically your recommendation to use the established definitions for sepsis used by CMS. My confusion is the following. I will see on a regular basis young adults, for example, a 21 year old male complaining of fever and sore throat and noted to have a heart rate >90 bpm. After examination if appropriate, I will perform a rapid strep test. Assuming the strep test is positive I will tell him he has strep throat and treat him accordingly. However he meets the CMS guideline for sepsis, is his correct diagnosis strep throat with sepsis?? I am reluctant to use sepsis in this scenario since I am accustomed to associating sepsis with patients who display evidence of clinical or hemodynamic instability (requiring resuscitative intervention) which this young man does not have nor need. Any clarification or insight you can provide would be greatly appreciated!