COVID-19 has changed life for emergency physicians on the front lines who are risking their own lives to combat the disease.
Explore This Issue
ACEP Now: Vol 39 – No 10 – October 2020ACEP has been actively advocating on your behalf to provide you with the tools and resources you need to safely do your job during the COVID-19 public health emergency. As part of that effort, ACEP staff, in conjunction with a subgroup of the ACEP Reimbursement Committee, designed a survey to help inform our advocacy strategy. The survey included 24 questions about the financial impact that COVID-19 has had on emergency medicine group practices and individual emergency physicians.
We received 197 responses, representing all emergency medicine group practice structures, group sizes, and historic volumes from across the country. The data confirmed anecdotal stories of the impacts on emergency medicine group practices, with almost all respondents reporting issues with the lack of reliable personal protective equipment and decreased volume and revenue.
Key findings on ED volumes and revenue are shown below.
ED Volume and Revenue Decreases, March–June 2020 vs. March–June 2019

Many emergency medicine group practices were forced to make workforce, coverage, and benefit changes:
- 21% have had to lay off physicians
- 31% have had furloughed physicians
- 56% of groups have cut pay for the same work
- 83% have experienced a decrease in productivity
- 83% of groups have cut hours of ED coverage
- 47% of groups have deferred or cut benefits
68% of emergency medicine group practices have had to provide or supplement personal protective equipment (PPE)
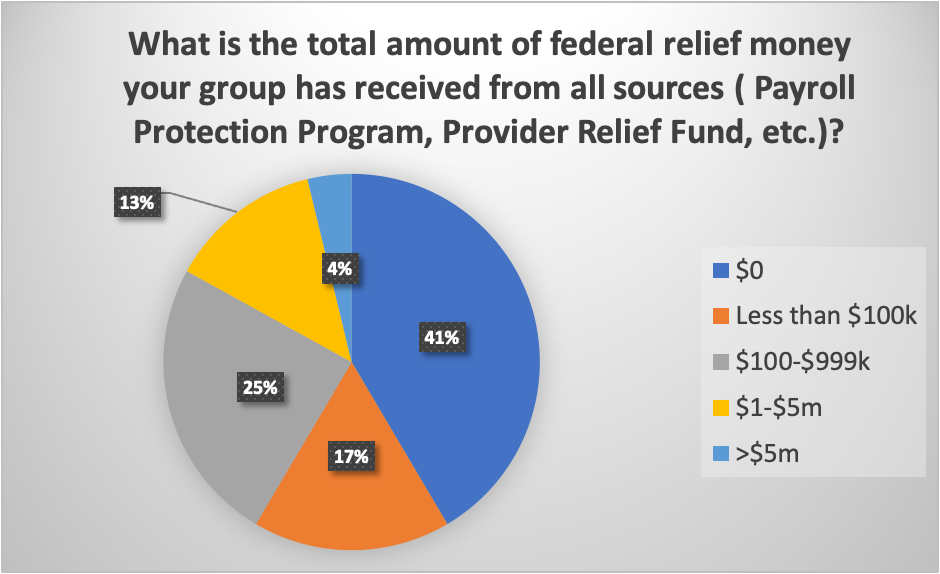
Emergency medicine groups are not getting the financial support they need:
- 21% of groups have asked their hospital for assistance, but of those, only 9% have received assistance.
- 36% of groups reported that their hospital has reduced stipends or support over the past three months.
- Of those that did received federal funds, 73% said it did not meet their financial needs.
Many emergency medicine groups are uncertain about the future:
- 44% of groups have concerns about their viability over the next four months
- 64% expect to decrease pay or benefits in the next six months
- 17% expect their hospital partners to declare bankruptcy in the next six months
The responses on the financial or economic impact of ED groups are concerning. At the conclusion of the survey, ACEP also asked an open-ended question about how COVID-19 has impacted the respondent personally. Although we cannot share actual responses, here are the general themes along with subcategories of concern we received:
- Family
- Can’t safely interact with family members—especially small children.
- Miss family—moved out of house into a hotel or apartment for foreseeable future or self-quarantined.
- Absence of touch—can’t hug family members, make them meals, etc.
- Financial strain—supporting more or all of family members with finances due to spouse or child laid off from work.
- Safety
- Almost 9 out of 10 respondents said they had difficulty locating PPE.
- More than 30 commenters complained their hospital/group showed little to no incentive to provide adequate PPE.
- The most frequent comment in the survey was that physicians are afraid of getting infected due to inadequate PPE or exposure.
- Hospital/group required self-quarantine procedures were not always followed or enforced consistently.
- Stress
- PPE donning and removal created decreased productivity among staff.
- Lost income due to loss of revenue created strained physician-hospital relationships
- No thanks from group/hospital/public for contributions made.
- Pushed to retire due to layoffs, age, or other reasons.
- Money
- Losing hours or other compensation—the second most frequent issue mentioned was lost hours, benefits, etc.
- Work more, less money—a majority reported working additional hours for less pay or no pay.
- Bankruptcy of group—about a quarter indicated they face layoffs or worse because of their group’s finances.
- Supporting family members—many reported family or personal money issues.
The survey results demonstrate how stressful the COVID-19 pandemic has been on emergency physicians and their families beyond simply the hardships of having to care for their patients. ACEP provides robust resources for both clinical and administrative assistance at https://www.acep.org/covid-19.
Some of our early advocacy efforts were described in an ACEP Now article in May, including our work with the Centers for Medicare & Medicaid Services to provide you with more regulatory flexibility (such as allowing you to perform medical screening exams via telehealth); our attempts to secure additional funding for emergency physicians from the Provider Relief Fund; and the steps we have taken to help improve your access to mental health treatment.
ACEP has had weekly conversations with the Centers for Disease Control and Prevention to discuss best clinical practices, share experiences from the ground, and hear more about current or upcoming guidance that could impact you and your patients.
We have also shared your stories about ongoing struggles obtaining PPE or being able to use your own PPE without fear of reprisal with the Occupational Safety and Health Administration (OSHA), The Joint Commission (TJC), and the American Hospital Association. We met with the TJC in March prior to the Commission issuing a statement that supports your right to bring your own PPE to work when your health care organization can’t routinely provide it. While the TJC statement was helpful, we are still hearing painful PPE-related stories from you—similar to the ones from the survey, and therefore have recently asked OSHA for a meeting to further discuss your concerns.
The survey reaffirms our need to continue fighting for you every day. We have created, and are continually updating, a list of advocacy priorities that guide our daily work.
Pages: 1 2 3 | Multi-Page




No Responses to “ACEP Surveys Members About COVID-19”