 As part of its ongoing commitment to providing the highest quality of emergency care, ACEP has developed the Clinical Emergency Data Registry (CEDR). This is the first emergency medicine specialty-wide registry at a national level, and it’s designed to measure and report health care quality and outcomes. It will also provide data to identify practice patterns, trends, and outcomes in emergency care. CEDR is an evolving registry that will support emergency physicians’ efforts to improve quality and practice in all types of EDs even as practice and payment policies change over the coming years. ACEP CEDR has been qualified by the Centers for Medicare & Medicaid Services (CMS) as a qualified clinical data registry (QCDR) to help emergency physicians and clinicians meet both the CMS Physician Quality Reporting System (PQRS) reporting and other quality reporting requirements.
As part of its ongoing commitment to providing the highest quality of emergency care, ACEP has developed the Clinical Emergency Data Registry (CEDR). This is the first emergency medicine specialty-wide registry at a national level, and it’s designed to measure and report health care quality and outcomes. It will also provide data to identify practice patterns, trends, and outcomes in emergency care. CEDR is an evolving registry that will support emergency physicians’ efforts to improve quality and practice in all types of EDs even as practice and payment policies change over the coming years. ACEP CEDR has been qualified by the Centers for Medicare & Medicaid Services (CMS) as a qualified clinical data registry (QCDR) to help emergency physicians and clinicians meet both the CMS Physician Quality Reporting System (PQRS) reporting and other quality reporting requirements.
Explore This Issue
ACEP Now: Vol 34 – No 05 – May 2015Quality Care Through Comparative Evidence
CEDR will, for the first time, enable emergency physicians to review their practice patterns and outcomes in comparison with their peers. Starting in 2015, CEDR will provide emergency physicians and clinicians with patient outcomes and health care quality metrics at the physician, ED, and group levels. Initially focusing on ACEP’s Choosing Wisely recommendations and ED throughput, CEDR will gradually expand to include other aspects of emergency care in 2016.
A Physician-Friendly System
CEDR is designed to be physician friendly. With little data entry burden to emergency clinicians or ED staff, clinical and patient data will be extracted, transformed, and loaded into CEDR from the ED’s electronic health record system, revenue cycle management system, or administrative data system (see Figure 1).
How Will CEDR Data Be Used?
The use of de-identified aggregated data generated by CEDR will support national comparative benchmarks, evidence-based shared decision making, and guideline-informed physician practices. It will provide participating emergency clinicians with feedback regarding their individual- and/or ED-level performance on a range of process and outcome quality measures, benchmarked against their peers at national and regional levels. For government policy makers, CEDR will provide further understanding around clinical effectiveness, patient safety, care coordination, patient experience, efficiency, and system effectiveness.
Why Should Emergency Physicians Participate in CEDR?
Instead of miring physicians in an alphabet soup of reporting requirements, CEDR allows for a single data capture to fulfill the requirements of multiple programs, making quality measure reporting more efficient. The health care environment is transitioning from volume-based to value-based payment for care. CEDR will ensure that emergency physicians, rather than other parties, are identifying what practices work best and for whom.
Privacy Policy
Information collected by CEDR is stored in a segregated HIPAA-compliant server in a secure electronic vault with robust backup. Only participating emergency clinicians or their designated ED administrator can see their performance with comparisons to national statistics.
Summary
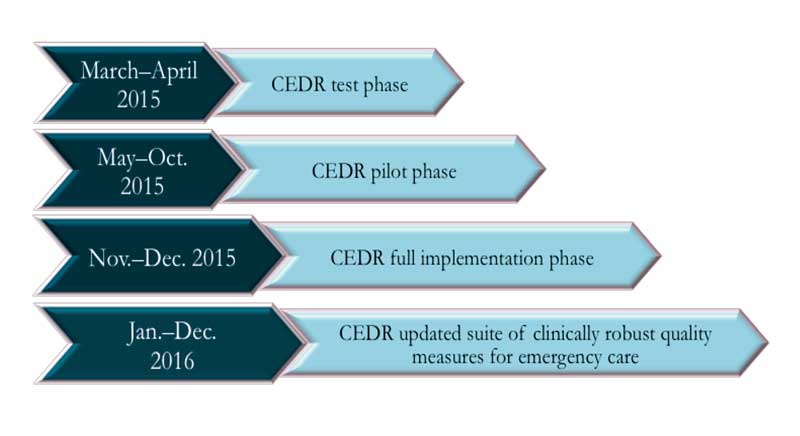
CEDR is being developed under a sophisticated information technology infrastructure and will be implemented in phases over the next year in terms of the number of participating EDs, scope, and functionality.
The initial testing and QCDR approval phase began in April 2015 with the participation of five EDs. The pilot phase is expected to begin in May 2015. Through the aggregation and organization of data on clinical effectiveness, patient safety, care coordination, patient experience, efficiency, and system effectiveness, CEDR will provide clinicians with a definitive resource for informing and advancing the highest quality of emergency care.
Dr. Augustine is director of clinical operations at EMP in Canton, Ohio; clinical associate professor of Emergency Medicine at Wright State University in Dayton, Ohio; and on the ACEP Board of Directors. Dr. Epstein is an attending physician in the Department of Emergency Medicine at Beth Israel Deaconess Medical Center and assistant professor of emergency medicine at Harvard Medical School in Boston. Dr. Granovsky is president of LogixHealth, an ED coding and billing company, andcurrently serves as the course director of ACEP’s Coding and Reimbursement courses. Ms. Jones is director of quality and health information technology in the public affairs division of ACEP in Washington, D.C.
Pages: 1 2 | Multi-Page






No Responses to “ACEP’s Clinical Emergency Data Registry to Measure, Report Health Care Quality, Outcomes”