
Case
A 44-year old woman with a peanut allergy accidently eats a cookie containing peanuts while attending her office holiday party. She arrives to the emergency department covered in hives, hypotensive, short of breath, and vomiting. She is diagnosed with anaphylaxis and treated successfully with epinephrine, nebulized beta-agonists, and H1 and H2 receptor antagonists as per the Guidelines for the Diagnosis and Management of Food Allergy in the United States.1
Explore This Issue
ACEP Now: Vol 33 – No 12 – December 2014Question
How long do you observe such patients, and what is the incidence of clinically important biphasic allergic reactions?
Background
Anaphylaxis is one of the most serious medical problems that can present to the emergency department. There are guidelines available to help clinicians assess and manage these life-threatening conditions.2
There is a fear in emergency medicine that patients can have a biphasic reaction. That is when the symptoms of anaphylaxis reoccur after being successfully treated.
Previous research has suggested the rate of biphasic reactions can be as high as 20 percent. This has led some experts to suggest observing patients with anaphylaxis for up to 24 hours.3 However, the literature shows that biphasic reactions can happen in a few minutes or even days later.
It is not practical to admit patients for up to one week of observation. So how long should you observe someone with an anaphylactic reaction, and what are the chances of a clinically important biphasic reaction?
Population: Adults (age >17 years) presenting to two urban EDs with allergic reactions
Intervention: Retrospective chart review
Control: N/A
Outcome: Primary (biphasic reaction) and secondary (mortality)
Excluded: <17 years old, primary diagnosis was asthma with allergy as secondary diagnosis, patient left ED prior to treatment, or patient had preexisting condition of angioedema
Authors Conclusions: “Among ED patients with allergic reactions or anaphylaxis, clinically important biphasic reactions and fatalities are rare. Our data suggest that prolonged routine monitoring of patients whose symptoms have resolved is likely unnecessary for patient safety.”
Key Results
There were a total of 428,634 ED visits over five years, with 2,323 (0.6 percent) considered allergic reactions and 496 (0.1 percent) classified as anaphylactic. Of these 2,819 patients, 185 had at least one subsequent visit for allergic symptoms (bounce back).
Five patients (0.18 percent) were identified as having clinically important biphasic reactions (95% confidence interval [CI], 0.07% to 0.44%). Two of these reactions occurred during the ED visit and three postdischarge (28 hours, 35 hours, and 143 hours). There were no fatalities (95% CI, 0% to 0.17%).
EBM Comments
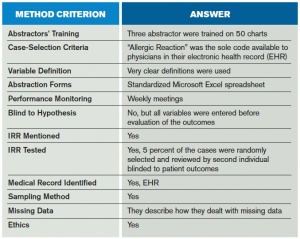
This was a very well-done retrospective chart review of consecutive adult patients presenting to the ED with allergic reaction or anaphylaxis (see Table 1). They followed the methods described by Gilbert et al and Worster et al.4,5
The study is limited by the retrospective nature. There was no defined protocol for managing allergic reactions. Some patients may have been missed if they presented to their primary care provider or left the province. There also could have been patients miscoded as shock on their second presentation rather than allergic reaction.
Bottom Line
Prolonged observation is likely unnecessary in patients whose symptoms resolve with therapy in the ED. Biphasic reactions are rare and can occur anywhere from 10 minutes up to six days after an initial reaction.
Case Resolution
The woman is observed for three hours after being treated for her anaphylactic reaction. She is doing well, with no vomiting, no shortness of breath, and resolving hives. She is discharged home with an epinephrine auto injector and oral corticosteroids, told to avoid triggers, and given an allergic reaction tool kit.6
Thank you to Anand Swaminathan MD, MPH, assistant program director in the department of emergency medicine at NYU/Bellevue Hospital for his help with this review.7
Remember to be skeptical of anything you learn, even if you learned it on The Skeptics Guide to Emergency Medicine.
 Dr. Milne is chief of emergency medicine and chief of staff at South Huron Hospital, Ontario, Canada. He is on the Best Evidence in Emergency Medicine faculty and is creator of the knowledge translation project the Skeptics Guide to Emergency Medicine (www.TheSGEM.com).
Dr. Milne is chief of emergency medicine and chief of staff at South Huron Hospital, Ontario, Canada. He is on the Best Evidence in Emergency Medicine faculty and is creator of the knowledge translation project the Skeptics Guide to Emergency Medicine (www.TheSGEM.com).
References
- Guidelines for the diagnosis and management of food allergy in the United States. J Allergy Clin Immunol. 2010;26:S1-58.
- Simons F, Ardusso L, Bilò, M, et al. World Allergy Organization Guidelines for the assessment and management of anaphylaxis. Curr Opin Allergy Clin Immunol. 2012;12:389–99.
- Tole JW, Lieberman P. Biphasic anaphylaxis: review of incidence, clinical predictors and observation recommendations. Immunol Allergy Clin N Am. 2007;27:309-26.
- Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: where are the methods? Ann Emerg Med. 1996;27:305-8.
- Worster A, Bledsoe RD, Cleve P, et al. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45:448-51.
- Anaphylaxis tool kit. Available at: https://www.allergicreactiontoolkit.com. Accessed Nov. 18, 2014.
- Rezaie S. Episode 1. REBEL-EM Cast. Available at: http://rebelem.com/rebelcast-episode-1. Accessed Nov. 18, 2014.
Pages: 1 2 3 | Multi-Page




2 Responses to “Biphasic Allergic Reactions: Observation, Treatment Guidelines”
January 26, 2015
biphasic allergic reactions… | DAILYEM[…] via this recent ACEP Now article by Dr. Milne […]
December 9, 2015
EllenHi Ken Milne, MD,
Thank you for sharing your knowledge on how to observe Biphasic Allergic Reactions and also for giving treatment guidelines for it.
This is really a great and helpful article.