
The hardest part of change is being convinced of its need. Patient satisfaction (experience of care) is a topic that rarely elicits positive emotions from providers. When tasked with improving my own scores, I began the journey with a great deal of skepticism. Before exploring how to improve, I had to first convince myself why this was necessary and worthwhile.
Explore This Issue
ACEP Now: Vol 35 – No 04 – April 2016I felt I was doing a good job as a doctor. My patient satisfaction scores were low, but in my mind, they were unimportant and outside of my control. Surveys had poor statistical power. Patients had unrealistic expectations and were often drug seeking, and the nature of the emergency department prevented my success.
These, among numerous other fallacies, were preventing me from becoming a better physician. To quote Mark Twain, “It’s not what you don’t know that kills you, it’s what you know for sure that ain’t true.”
As I challenged myself, many things surfaced that I had not considered.
Patient experience has direct financial implications for physicians. A tenet of good business is that consumers vote with dollars. One bad experience may influence friends, family, and, if documented on social media, even thousands of future patients.
Time spent at bedside does not equal better care. High-quality communication takes no additional time when interactions are focused and address patient expectations.
Physicians drive patient satisfaction. Skilled, empathetic communication influences experience greater than any single variable. Improved clinical outcomes and lower ED recidivism rates are valued dividends.
First Steps of Change
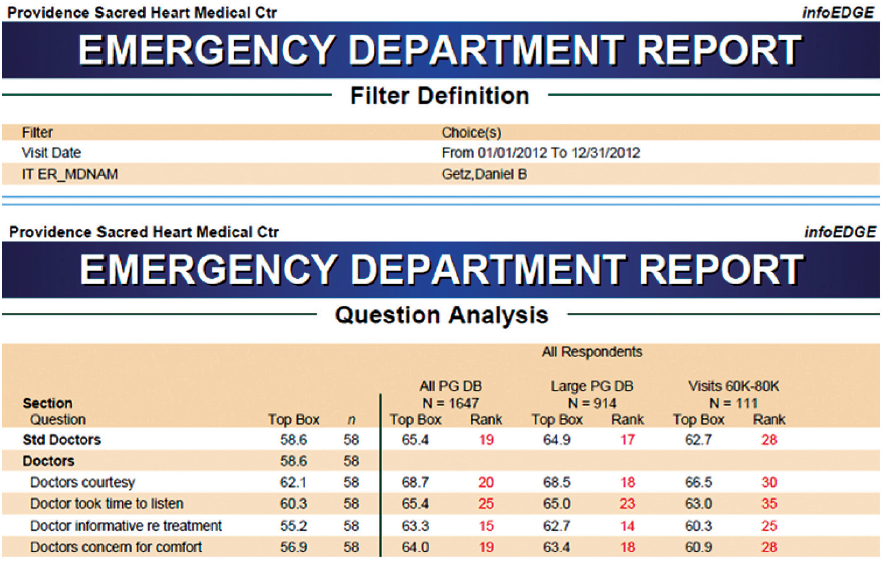
After several nights of fractured sleep, I scheduled a meeting with our service excellence manager to review my data. I learned that I was below the 30th percentile for the majority of metrics (see Table 1).
As a medical director, I could not effectively lead my department without improving my own practice, so I began to study the many variables that drive patient perception.
It became apparent that I was not communicating effectively. My unintentional lack of collaboration with patients made it impossible to deliver reassurance and emotional comfort and alleviate fear. Any effective approach must set reasonable expectations. We serve as clinicians and guides, helping patients navigate the terrifying and often foreign ED journey. Without providing context or framework for their stay, we inadvertently foster unrealistic patient expectations. This is the reason approaches such as AIDET work.
AIDET Method
Acknowledge and Introduce: This sets the stage for patient experience. Knock, and wait for permission to enter. Greet everyone in the room, and reciprocate with your name and title. Make routine eye contact, and use receptive body language. If they have waited, let them know their time is important by apologizing. I may be having an incredibly stressful shift, but my goal is for patients to feel that I am 100 percent focused on them at that point in time.
Always sit. Patients perceive that you spend more time when you sit, and it implies interest. Communication is a team sport. Utilize active listening, allowing patients the opportunity to fully describe their symptoms. Shared experiences or interests help to build rapport. Friendly conversation is a great tension diffuser.
Duration/Describe: Develop reasonable goals with patients, including a reasonable estimate of time they will spend in the department. Discuss conditions in your differential diagnosis, and inform them that your role is to exclude life-threatening illness. Initiate dialogue surrounding realistic pain management, engaging them as a partner in their care. For example: “Mrs. Jones, I know your pain is a 10 and reaching a 0 for you today is unlikely, but let’s aim for a 4. We are going to get you more comfortable.”
Discuss that they may leave the ED without a formal diagnosis; for many, we are the “what it ain’t” department. Visit with your patients frequently, even if only popping your head in to update them on progress, results, or unanticipated delays. Patients with benign chest pain believe they are having a heart attack and will be reassured by their normal results. Don’t make patients wait until the end of their stay to hear good news.
Explain and Engage: This is the most important part of the patient encounter. Using simple terminology, review with your patients what you have ordered, have or have not found, follow-up and treatment recommendations including symptoms of concern, and all new prescriptions. Finally, and this is the easiest to forget, provide everyone an opportunity to ask questions: “I would like to take a moment to try and answer any questions that you or your family/friends may have.” As medical director at a 90,000-plus visit ED, I spend a fair amount of time in complaint resolution meetings, and I would estimate that nearly all of the complaints of merit could have been avoided if providers spent more time on this step.
Thank: At the end of the visit, take a moment to genuinely thank your patients for the opportunity to care for them. Patients should feel valued. I am humbled by the amount of trust patients place in my hands, and at the close of a visit, I want them to know that I am sincerely thankful for the opportunity to provide their care.
The Benefits of Focusing on Patient Experience
As I became better versed in these techniques, my job satisfaction unexpectedly and substantially improved. Cookies were delivered to the department by sweet little old ladies. Notes of thanks began to come in routinely as well as requests to become a patient’s primary care provider (a patient’s highest form of praise). With a heightened sense of pride in my practice and continued efforts, I was able to obtain sustainable results.
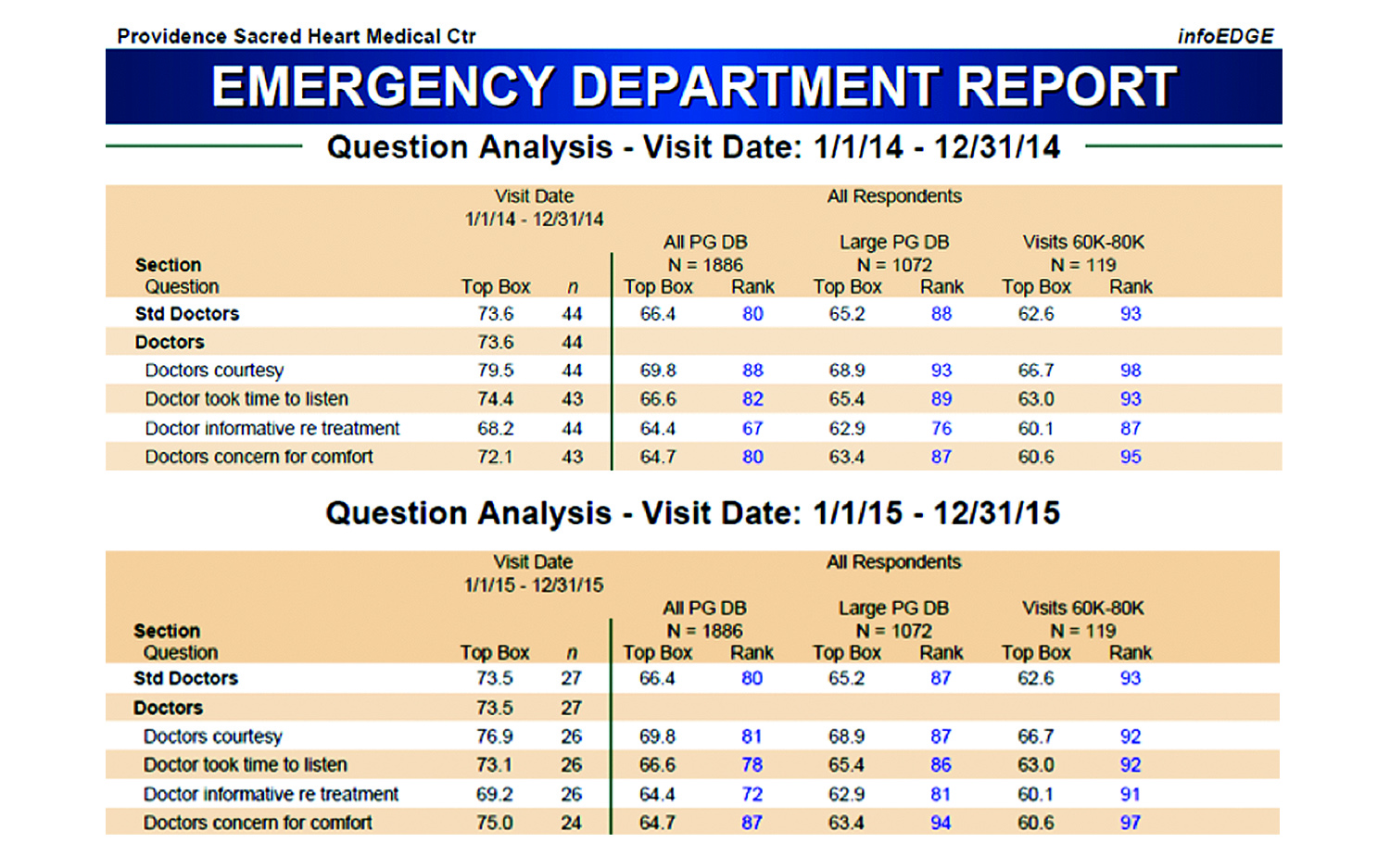
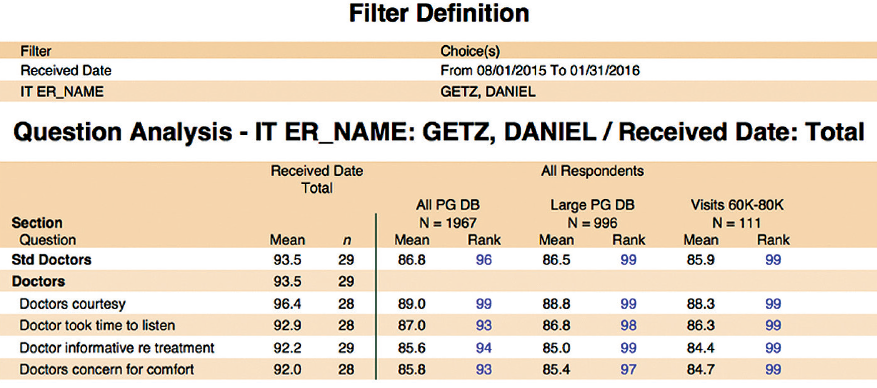
Over the course of six months, my patient experience scores climbed from the 20th percentile to the 90th and have held steady for the past two years (see Tables 2 and 3). With myself as a case study, I was ready to engage my physician partners, many of whom also had been unaware they were struggling.
I am glad to report that our ED has made significant gains in patient experience and our providers continue to improve. More important, this has elevated the morale of everyone on our team. Enhancing patient experience does not need to invoke feelings of fear or hostility. It is simply better patient care.
 Dr. Getz is ED medical director at Providence Sacred Heart Medical Center in Spokane, Washington; founder of Satisfaction Statistics, Inc., a patient satisfaction survey and patient experience consulting company; and adjunct clinical instructor for the department of emergency medicine at the University of Washington.
Dr. Getz is ED medical director at Providence Sacred Heart Medical Center in Spokane, Washington; founder of Satisfaction Statistics, Inc., a patient satisfaction survey and patient experience consulting company; and adjunct clinical instructor for the department of emergency medicine at the University of Washington.
Pages: 1 2 3 | Multi-Page




5 Responses to “Boost Patient Satisfaction Scores, Become a Better Doctor”
April 29, 2016
M LynchCan you say “I drank the kool aid” or “conflict of interest? The author doesn’t point out, until the end of the article, that he has his own patient satisification consulting firm…so yeah, he has a big financial incentitive in surveys!
I often sit down with patients, explain things, answers tons of questions. I also, works in Urgent Care. Patients are all in rooms, not lined up in the hallways. No one is handing me EKGs showing STEMIs, alerting me to a code coming in, a patient seizing, a consult or radiology on the phone. I also get 10 minutes to eat lunch, have access to a clean and safe bathroom and am not pressured or encouraged to prescribe unnecessary antibiotics or narcotics. I don’t have to make sure I meet criteria for door to doc time, door to cath, door to TPA. I miss it, but I refuse to be treated like a retail employee instead of a doctor.
Dr. Gertz. Instead of paying you to tell me how to do my job how about we work on making the ER staff happier and making their jobs easier. Make sure your staffing in optimal and safe, have people around (not the clinicians) responsible for “guest relations.” Invest money in the hospital, instead of useless and harmful surveys. Make more private rooms with TV’s and get more chairs (I often couldn’t find one to sit at to do my endless charting), put a white board in every room with dr’s name, RN’s name, what patient is waiting for and when they should expect it to happen (add an hour). Don’t require any doctor seeing high acuity patents to see boo-boos and colds. Never have a doctor alone on a night shift. Hire more midlevels. Make sure everyone EATS! Has access to water and clean bathrooms and can go, I spent many a 12 hr shift hangry, thirsty and in agony because I had not gone to the bathroom…once.
Let us see our surveys. At my last job I was told my scores were low. I asked how many surveys I had gotten and to see them. I was told I four and one was negative…something to do with being rushed and frequently interrupted. Firstly this is not enough surveys to be statistically significant, second how am I to learn if I can’t see my surveys? Oh, the “bad” one was from a horrible overnight when I was alone. I ran three codes, got a stemi to the cath lab in 11 minutes and help a family decide to withdraw care. Shame none of them got surveys. The “patient satisfaction” consultant told me to tell people when I was discharging them that “you may receive a survery about your experience, please give me all 5’s.” I refused. “Sorry about your 2nd miscarriage this year, could you make sure you rate your experience a 5?” If you have never touched a patient don’t tell me how to do my job.
Pay me 1/5 of what you pay for these useless surveys, I will tell you how to make EVERYONE in the ED happy.
Also wondering what happened to all the really sick patients that the author was not seeing, as he was focusing on his scores. Would be nice to see his morbidity and mortality numbers during this time. Studies show all these metrics rise with increased scores.
May 9, 2016
Mark BuettnerThank You Dr. Lynch. You are Spot On Sir!
May 15, 2016
Thomas CarterI saw over 2000 patients and had 7 scores the last time I looked. I got more patients bringing me unsolicited food for a job well done then even got a chance to answer surveys
To say the are statistically weak is a foolish statement. They are invalid.
May 30, 2016
Jerry W. Jones, MD FACEP FAAEMTo me, patient satisfaction surveys should reflect more objective data: “What time did you check in? What time were you first seen by the physician? How much time did the physician spend with you? Did the physician perform a physical exam? Did the physician acknowledge those accompanying you? Did the physician discuss your (presumptive) diagnosis with you? Did the physician explain his/her plan for your care? Did the physician allow you to provide elements of your history yourself? Did the physician give you an opportunity to ask questions? Did the physician return to check on you personally during your stay in the emergency department?”
Unfortunately, hospital administrators use patient satisfaction surveys as hammers over the heads of physicians and nurses who work in the emergency department. And they do this not by asking objective questions, but instead “Did you get what you wanted?” Patient surveys aren’t being used for the improvement of patient care – they are being used to deny pay raises, bonuses or to negotiate down emergency group contract extensions. It didn’t take the administrators long to realize that they could easily skew the responses on the patient satisfaction surveys from the emergency department simply by creating a delay in moving admitted patients out of the ER.
Have you ever taken a CUSTOMER survey before? Did any of them ask if you thought you should have been charged less for the product you purchased or if you thought that the product should have been of better quality? No! The provision of medical care based on training and experience is NOT a PRODUCT.
As physicians we must do what is best for our patients and that means that we can’t always tell them just what they want to hear or prescribe medication that is not in their best interests. I find it so ironic that on the one hand physicians are being castigated as the “cause” of an opioid-abuse epidemic but on the other hand they are basically being told that if they stop prescribing opioids to patients who want them they will get bad patient satisfaction surveys and their staff privileges could be in serious jeopardy.
May 30, 2016
NNIt never ceases to amaze me how medical leadership does not or refuses to acknowledge the significance of the physical and mental well-being of their medical staff and its effect on patient surveys as well. Improving scores should not simply rest on the AIDET model, of which I subscribe. Doctors are people and people matter. Shouldn’t their happiness and satisfaction matter as well?
I made a personal decision 8 years ago to leave full-time emergency medicine because of its focus on the business without regard for the “workers”. Although I was productive and my billing was impeccable, I had poor patient satisfaction scores. The pressure to improve my scores without my leadership offering any tools to do so was immense. Then I had an epiphany, the leadership did not possess the skills to address anything as personal as the well-being of the physicians. Instead, the unspoken threat of losing one’s job if no or minimal improvement was made hung in the air like a black cloud. A negative incentive to improve. All this did was create resentment. After leaving I performed a self-evaluation and made a decision. My priority would be patient first, documentation second and the speed at which I saw patients, third. Then I would work part-time and only when I wanted. I could care less about surveys. Although my income has dropped dramatically, I’m much happier. Number of patient complaints in 8 years? Less than 10. Happy patients return and bring their money with them. Despite the pressure to speed up at times, there is no proof that this alone improves quality of care. In fact, it decreases it. I have never been fired from any job. Why? My billing and documentation remain impeccable and I have minimal if any patient complaints. The companies for whom I work still have no regard for its workers, including me. But I make money for the company and money talks.