Case
A 40-year-old female at 11 weeks, five days gestation presented to the emergency department (ED) with concern for lower abdominal pressure and inability to fully empty her bladder. She had urinary dribbling when standing and leaning forward. She denied fevers, back pain, saddle anesthesia, numbness, or weakness in the extremities. She reported no history of prior back surgeries, intravenous drug use, recent falls, trauma, or known inciting event. There was no vaginal bleeding or vaginal discharge. Transvaginal ultrasound (TVUS) performed in the outpatient setting a couple of weeks prior to presentation confirmed an intrauterine pregnancy (IUP) with a retroverted uterus. Straight catheterization resulted in approximately 1,500 mL of clear urine output and relief of symptoms. Urinalysis showed no evidence of infection, and the patient was discharged home.
Explore This Issue
ACEP Now: Vol 43 – No 01 – January 2024The patient returned the next day with concern for ongoing urinary retention. She had only been able to void small amounts since the prior visit. Foley catheterization was again performed with approximately 1,200 mL of urine output and relief of symptoms. The obstetrics team was consulted due to the urinary retention. The cervix was not visualized during pelvic examination, but manual examination identified the cervix tucked under the pubic bone in an anterior position, concerning for an incarcerated gravid uterus (IGU). The patient was admitted to the obstetrics service and underwent spinal anesthesia in the operating room to manually reduce the uterus. A pessary was inserted during that procedure. On the next day, the Foley catheter was removed and the patient was able to spontaneously void. She was discharged in stable condition with close follow-up.
Analyzing a Rare Diagnosis
Incarcerated gravid uterus is a rare diagnosis with an estimated incidence of one in 3,000 to one in 10,000 pregnancies.1-3 It most commonly occurs in patients with a retroverted uterus during weeks 10 through 16 of pregnancy. As the uterus grows, it can spontaneously correct; however, if the uterine fundus remains in the pelvis it can become trapped against the sacral promontory while the cervix is trapped against the pubic symphysis.1,4 Approximately 15 to 20 percent of all pregnancies occur in a retroverted uterine position, however only a rare minority of those pregnancies lead to IGU.1,5
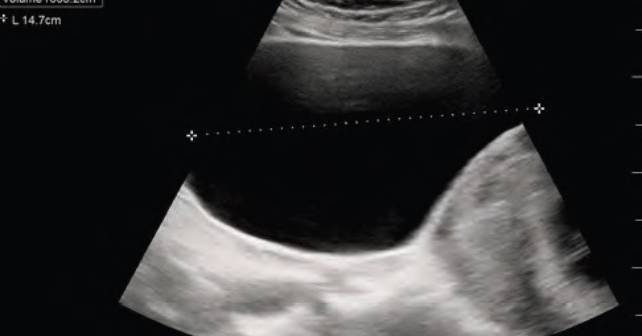
Risk factors include prior abdominal surgeries, history of pelvic inflammatory disease, or prior history of uterine incarceration.6 IGU can be identified via history and physical, pelvic examination, or MRI. Alternatively, ultrasound can be utilized as a diagnostic modality. Transabdominal ultrasound is more helpful for IGU diagnosis than TVUS as the transabdominal approach allows for better visualization of the cervix in relation to the uterus.5,7 Since IGU is a rare presentation, the literature primarily consists of case reports and case series. Treatment options include Foley catheterization until the uterus spontaneously reduces and adopts a normal vertex presentation, having the mother adopt a knee-to-chest position, or manual reduction with appropriate pain control. More invasive techniques such as colonoscopic or laparoscopic reduction have been described.1,7
Obstetrics Consultation
Given the rare presentation, the authors submit that acute urinary retention in a pregnant patient without clear identifiable cause (history of neurogenic bladder, recent medications with anticholinergic side effects, cauda equina signs or symptoms, etc.) should lead to obstetrics consultation. In addition, while abdominal MRI and/or ultrasound may aid in the diagnosis of IGU, this should not delay care. Bladder decompression and obstetrics consultation should be prioritized.
The decision to reduce the uterus should be made by the obstetrics specialist. Maintaining a high level of suspicion for this rare diagnosis will help establish early identification and treatment, therefore reducing risk of maternal and fetal complications.2
 Dr. McKinley completed Emergency Medicine ultrasound fellowship at Maine Medical Center and is currently the Assistant Director of Point of Care Emergency Ultrasound with the Miami Valley Emergency Specialists in Dayton, Ohio. She is a clinical faculty associated with the Wright State University Emergency Medicine Residency.
Dr. McKinley completed Emergency Medicine ultrasound fellowship at Maine Medical Center and is currently the Assistant Director of Point of Care Emergency Ultrasound with the Miami Valley Emergency Specialists in Dayton, Ohio. She is a clinical faculty associated with the Wright State University Emergency Medicine Residency.
 Dr. Bauman completed an Emergency Medicine ultrasound fellow at Maine Medical Center and is currently the Co-Director of Ultrasound at Southern Maine Health Care Medical Center where he practices as an attending physician.
Dr. Bauman completed an Emergency Medicine ultrasound fellow at Maine Medical Center and is currently the Co-Director of Ultrasound at Southern Maine Health Care Medical Center where he practices as an attending physician.
 Dr. Christensen completed an emergency medicine Ultrasound fellowship at Maine Medical Center and is currently the director of Point of Care Ultrasound with Blue Water Health in Brunswick, Maine.
Dr. Christensen completed an emergency medicine Ultrasound fellowship at Maine Medical Center and is currently the director of Point of Care Ultrasound with Blue Water Health in Brunswick, Maine.
 Dr. Gaudet completed emergency medicine residency at Maine Medical Center and is currently a fellow in Emergency Department Quality & Management at Beth Israel Deaconess Medical Center. She is a Clinical Instructor associated with Harvard Medical School.
Dr. Gaudet completed emergency medicine residency at Maine Medical Center and is currently a fellow in Emergency Department Quality & Management at Beth Israel Deaconess Medical Center. She is a Clinical Instructor associated with Harvard Medical School.
 Dr. Wood is an associate professor of Emergency Medicine at Tufts University School of Medicine and an emergency medicine attending physician at Maine Medical Center
Dr. Wood is an associate professor of Emergency Medicine at Tufts University School of Medicine and an emergency medicine attending physician at Maine Medical Center
 Dr. Linnell is an Obstetrics and Gynecology attending physician at Maine Medical Center. She is a clinical instructor for Tufts University School of Medicine and is the co-site director of the Tufts University School of Medicine third year OB-GYN clerkship.
Dr. Linnell is an Obstetrics and Gynecology attending physician at Maine Medical Center. She is a clinical instructor for Tufts University School of Medicine and is the co-site director of the Tufts University School of Medicine third year OB-GYN clerkship.
 Dr. Wilson is an emergency medicine attending physician and director of Emergency Medicine Ultrasound Fellowship at Maine Medical Center.
Dr. Wilson is an emergency medicine attending physician and director of Emergency Medicine Ultrasound Fellowship at Maine Medical Center.
References
- Vidaeff A, Schneider K. Incarcerated gravid uterus. UpToDate website. Last updated November 23, 2022. Accessed December 8, 2023.
- Gardner C, Jaffe T, Hertzberg B, et al. The incarcerated uterus: A review of MRI and ultrasound imaging appearances. AJR Am J Roentgenol. 2013;201(1):223-9.
- Carney A, Tobler K, James K. First trimester uterine incarceration resolved with conservative management in a multifetal gestation. Obstetrics & Gynecology. 2019;133:122S-123S.
- Newell S, Crofts J, Grant S. The incarcerated gravid uterus: complications and lessons learned. Obstet Gynecol. 2014;123(2 Pt 2 Suppl 2):423-42.
- Ntafam C, Beutler B, Harris R. Incarcerated gravid uterus: A rare but potentially devastating obstetric complication. Radiol Case Rep. 2022;17(5):1583-1586.
- Tougas K, Hicks B, Mayersak R. Acute urinary retention: A rare case of incarcerated uterus in the gravid ED patient. EMResident website. Published June 10, 2022. Accessed December 8, 2023.
- Dai C, Peng J, Chen R. Acute urinary retention in the first-trimester of pregnancy: A case report. Cureus. 2022;14(3):e23057.
Pages: 1 2 3 | Multi-Page









No Responses to “Case Report: Acute Urinary Retention in a Pregnant Woman”