An inverted T wave occurring in an isolated electrocardiographic region is referred to as an isolated T wave inversion (TWI) or isolated T wave negativity.1 Such TWIs can occur in healthy individuals with no evidence of heart disease but are also seen in patients with coronary artery disease. In asymptomatic patients without cardiovascular history or risks, isolated TWIs are unlikely to indicate undiagnosed advanced coronary artery disease.
TWIs can be transient. Transient causes include hypokalemia, early stages of hypertrophic cardiomyopathy, hyperventilation, and transient ischemia from coronary vasospasm (people of Asian ethnicity also are more likely to have this latter finding).1 Even anxiety and fear have been described in association with transient TWI.
However, a study by Farhan et al assessing patients with chronic stable angina demonstrated that TWI in aVL correlated highly with significant left anterior descending artery (LAD) lesions, typically mid segment.2 Alarmingly, of the 14 percent of ECGs in this study that demonstrated this isolated finding, all were read as normal by referring physicians. But this finding should not be viewed as normal in the setting of chest pain, as it may be the first objective finding in an evolving ST-elevation myocardial infarction (STEMI).
Case Report
A 51-year-old man with asthma, hypertension, and hyperlipidemia presented with crushing substernal left-sided chest pain radiating down his left arm that started 10 minutes prior to arrival. He was seen immediately upon arrival by the triage physician, and his initial ECG (obtained at 7:50 p.m.) demonstrated isolated TWI in aVL (see Figure 1). In the setting of significant left-sided chest pain and the ECG finding, the patient was moved to the critical area of emergency department.
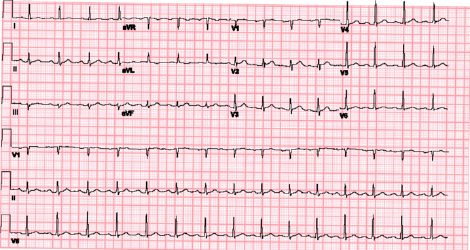
Figure 1: The patient’s initial ECG demonstrated isolated T wave inversion in aVL.
In the critical area of the department, the patient was clutching his chest and was diaphoretic. A repeat ECG (obtained at 8:03 p.m.) demonstrated ST elevation in V1–V3 with reciprocal ST depression in II and aVF (see Figure 2).
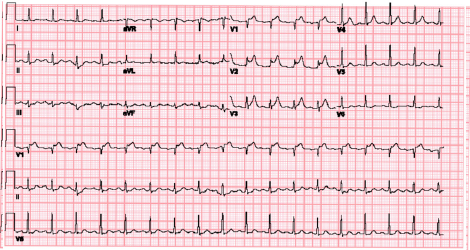
Figure 2: The patient’s repeat ECG demonstrated ST elevation in V1–V3 with reciprocal ST depression in II and aVF.
A “Code STEMI” was initiated. Bedside echo showed preserved left ventricular ejection fraction with akinesia of the antero-septal segment. The initial troponin was negative. Tenecteplase 50 mg was given at 8:16 p.m., with aspirin 325 mg, clopidogrel 300 mg, heparin 4,000 U bolus, and rosuvastatin 40 mg. Next, a heparin 12 U/kg/hr infusion was initiated. A subsequent ECG (obtained at 8:41 p.m) showed greater than 50 percent resolution of the prior V1–V3 ST elevations. The patient reported that his chest pain improved by 8:56 p.m. The patient was transferred to a percutaneous coronary intervention center. Catheterization was completed within 24 hours, demonstrating 99 percent occlusion of the LAD (see Figure 3).
Discussion
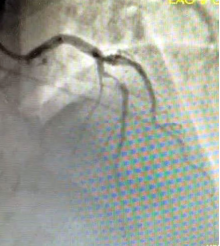
Figure 2: The patient’s repeat ECG demonstrated ST elevation in V1–V3 with reciprocal ST depression in II and aVF.
Images: Youstina Michael
An isolated TWI in aVL is not a well-recognized early sign of occlusion across the relevant medical specialties. In a survey by Hassen et al, only 25 percent of physicians identified an isolated TWI in aVL as abnormal, although emergency physicians were better than other specialties at recognition.3 This study demonstrated that angiograms done specifically during the evaluation for STEMI revealed mid-LAD lesion association with TWI with a sensitivity of nearly 88 percent, and positive predictive value (PPV) of 81 percent for mid-LAD lesions greater than 50 percent. Patients with similar ECG findings who underwent coronary angiography for other reasons demonstrated a sensitivity of 65 percent, PPV of 83 percent, and specificity of 67 percent for mid-LAD lesions 70 percent or greater. The LAD supplies a large portion of the heart and renders a large area of myocardium at risk in the setting of an occlusion, making this subtle ECG change important to identify.
For hospitals that do not have an on-site catheterization lab, thrombolytics may be required as a bridge to definitive therapy. (“Time is myocardium.”) Patients who receive thrombolytic therapy may have improvement in chest pain and ECG findings. However, these patients require cardiac catheterization within 24 hours of presentation. Early recognition and treatment of patients with concerning presentations and an isolated TWI in aVL may save a life.
Dr. Michael is an attending physician, Dr. Sokup is a resident, and Dr. Jeong is residency director and associate chair for education in the department of emergency medicine at Coney Island Hospital in Brooklyn, New York.
References
- Okada M, Yotsukura M, Shimada T, et al. Clinical implications of isolated T wave inversion in adults: electrocardiographic differentiation of the underlying causes of this phenomenon. J Am Coll Cardiol. 1994;24(3):739-745.
- Farhan HL, Hassan KS, Al-Belushi A, et al. Diagnostic value of electrocardiographic T wave inversion in lead aVL in diagnosing coronary artery disease in patients with chronic stable angina. Oman Med J. 2010;25(2):124-127.
- Hassen GW, Costea A, Carrazco C, et al. Isolated T wave inversion in lead aVL: an ECG survey and a case report. Emerg Med Int. 2015;2015:250614.
Pages: 1 2 | Multi-Page





No Responses to “Case Report: Subtle ECG Findings Evolving to STEMI”