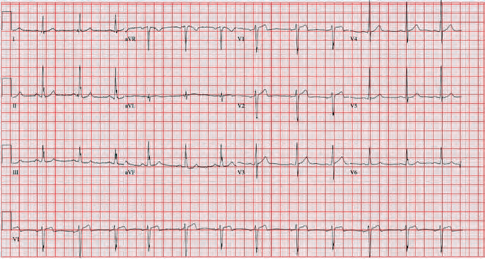
A 35-year-old male presented to the emergency department complaining of chest pain that started 1.5 hours prior to arrival. The patient had an EKG performed within 10 minutes of arrival while in triage (see Figure 1). In the absence of significant ST elevations, the EKG was signed and the patient was placed back in the queue to await a bed.
Explore This Issue
ACEP Now: Vol 43 – No 08 – August 2024Once placed in a treatment room, further history and physical examination are obtained. Two years prior, he had an NSTEMI requiring RCA stenting and is currently on dual antiplatelet therapy. He has prediabetes, hypertension, hyperlipidemia, and obesity. His vital signs were within normal limits. He appeared uncomfortable and slightly diaphoretic. His cardiopulmonary exam was unremarkable.
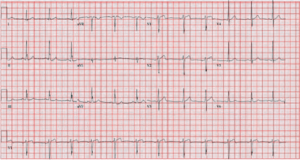
He was hospitalized two months prior and had a normal stress test. An EKG during that admission showed T-wave inversions in leads III and aVF (see Figure 2). These inversions have been present since his stent placement.
Diagnosis and Treatment
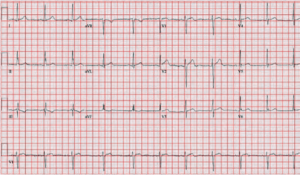
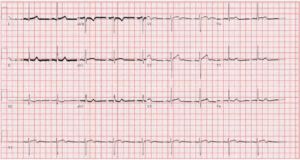
The patient was given aspirin, morphine, and nitroglycerin. He was pain-free and serial EKGs were performed showing a gradual return to his chronic inversion in lead III (see Figure 3). High-sensitivity troponins returned at 6 ng/L and 15 ng/L 1 hour apart (normal 0-20 ng/L). Given his EKG findings and presentation, he was started on heparin and admitted. His troponin peaked at 7,449 ng/L. One day after his initial presentation he was taken to the cath lab where it was discovered that he had severe in-stent restenosis of the RCA. He underwent balloon angioplasty with success and was subsequently discharged.
Discussion
The initial EKG performed demonstrated pseudonormalization of the T-wave in the presence of myocardial ischemia. Persistent T-wave inversions can occur for many different reasons such as underlying heart and pulmonary disease, persistent juvenile T-wave pattern, or for idiopathic reasons, amongst others. In the presence of ischemia, reversal of the inversions can occur. The relationship of this phenomenon to ischemia was first described in the 1970s in 38 patients where half displayed pseudonormalization of T-waves on stress test and half with anginal chest pain.1 The relationship was reconfirmed in several additional studies. It was later shown with continuous EKG monitoring that this process can occur when ischemia is present even in the absence of typical anginal symptoms.2
It has been suggested that these changes arise from the same mechanisms that create the hyperacute T-waves that can precede ST elevation MIs.3 Hyperacute T-waves arise from a shortening of the action potential in the ischemic myocardium which alters repolarization leading to increased T-wave amplitude in affected leads. When this process is superimposed on regions of the myocardium that have chronic ischemic changes, the effect is flattening and eventually positive T-wave transformation.
Pseudonormalization in the absence of the correct clinical context may not carry a high sensitivity nor positive predictive value. In a study looking at stress tests from 4,353 participants, 140 patients exhibited pseudonormalization but only 33 patients had a reversible perfusion defect on SPECT imaging.4 In a similar investigation of 50 patients noted a relationship between pseudonormalization and ischemia although the study was underpowered to meet clinical significance.5 Studies looking at this phenomenon in the emergency department setting for patients presenting with chest pain are lacking. Considering hyperacute T-waves have been accepted as STEMI equivalents, it is possible that pseudonormalization could gain more recognition as an indicator of ACS.6
This case shows the importance of close comparison of an active EKG to prior EKGs, especially without knowing the full clinical scenario. Having an understanding of the pseudonormalization of T waves should serve as another tool in our diagnostic toolbox when reviewing EKGs from triage can help expedite emergent department care. This can be used with other aspects of the clinical presentation to more effectively stratify the need for admission and cardiology consultation.
 Dr. Young is an emergency physician at Saint Francis Hospital and Medical Center, Hartford, Conn.
Dr. Young is an emergency physician at Saint Francis Hospital and Medical Center, Hartford, Conn.
References
- Noble RJ, Rothbaum DA, Knoebel SB, McHenry PL, Anderson GJ. Normalization of abnormal T waves in ischemia. Arch Intern Med. 1976 Apr;136(4):391-5.
- Chierchia S, Brunelli C, Simonetti I, Lazzari M, Maseri A. Sequence of events in angina at rest: Primary reduction in coronary flow. Circulation. 1980 Apr;61(4):759-68.
- Simons A, Robins LJ, Hooghoudt TE, Meursing BT, Oude Ophuis AJ. Pseudonormalisation of the T wave: old wine?: A fresh look at a 25-year-old observation. Neth Heart J. 2007;15(7-8):257-9.
- Loeb HS, Friedman NC. Normalization of abnormal T-waves during stress testing does not identify patients with reversible perfusion defects. Clin Cardiol. 2007 Aug;30(8):403.
- Fuentes Mendoza JA, Gonzalez Galvan LM, Guizar Sanchez CA, Pimentel-Esparza JA, Fuentes Jaime J, Cervantes-Nieto JA. Pseudo-Normalization of the T-wave during stress and its relationship with myocardial ischemia: Evaluation by myocardial Perfusion single photon emission computed tomography (SPECT). Cureus. 2023 May 2;15(5):e38428.
- Kontos, M, de Lemos, J. et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain in the Emergency Department: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022 Nov, 80 (20) 1925–1960.
Pages: 1 2 3 | Multi-Page





No Responses to “Case Report: The Not So Normal, Normal EKG”