Explore This Issue
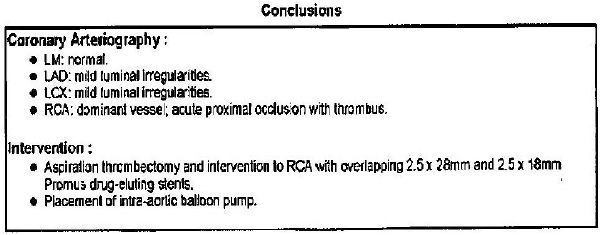
ACEP Now: Vol 41 – No 01 – January 2022Figure 1: Conclusions of the university catheterization lab.
Over the next day, she had increasing pressor requirements and additionally was determined to have a severe anoxic brain injury. Her hemodynamic condition continued to worsen, and as the family felt that continuing futile medical care was not in accordance with her wishes, she died within several minutes of switching to comfort-focused care.
The Lawsuit
The patient’s husband filed a lawsuit against the physician who discharged her. He sued the EMS service, alleging that dispatch took six minutes (as opposed to the policy of dispatch within two minutes). He sued both the EMT and paramedic who responded, claiming that they did not start CPR fast enough after arriving.
The allegations against the physician hinged on the fact that the patient had multiple risk factors for acute coronary syndrome and active chest pain and that only one troponin was obtained.
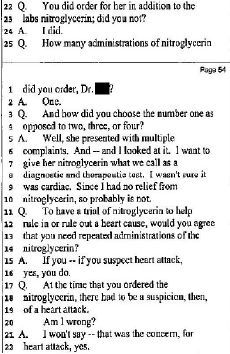
Figure 2: Excerpt from the physician defendant’s deposition.
The physician countered that her pain was burning, not heavy or pressure-like. He claimed that because it had been two to three hours since the pain started, only one troponin was necessary.
During the deposition, the plaintiff’s attorney focused on the patient’s response to receiving nitroglycerin. The doctor felt that since the patient did not have improvement of her pain, she was unlikely to have acute coronary syndrome (see Figure 2).
Ultimately, both sides agreed on a confidential settlement, and the lawsuit was withdrawn before it went to trial.
Discussion
This case illustrates why chest pain is such a high-risk area in emergency medicine. For many other complaints, a patient who is inappropriately discharged will have worsening symptoms over hours or days and have plenty of time to return to the emergency department and avoid catastrophe. Not so for chest pain. Sudden cardiac death leaves almost no opportunity for a second chance.
The development of the HEART Pathway decision aid and high-sensitivity troponins have significantly improved the care of chest pain patients since this case happened in 2011. This patient had a HEART score of 4 at a minimum (even with only giving her one point each for the history and ECG). This patient was not low-risk. Obtaining high-sensitivity troponins at arrival and two hours later likely would have revealed abnormalities that would have changed her care, although this is admittedly conjecture.
Ultimately, this case is a good reminder for emergency physicians to use the highly effective prognostic tools we have at our disposal. Not all major adverse cardiac events are avoidable, but appropriate application of these tools makes catastrophic outcomes very rare and provides an excellent defense when the unforeseeable happens.
Note: We do not yet have high-sensitivity troponins at my hospital. For a similar patient who presents with less than three hours of symptoms, we would perform three conventional troponins three hours apart (0h, 3h, 6h) prior to clearance for discharge from the emergency department.
To read the full medical record from this case, click here.
 Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice.
Dr. Funk is a practicing emergency medicine physician in Springfield, Missouri, and owner of Med Mal Reviewer, LLC. He writes about medical malpractice.
Pages: 1 2 3 | Single Page





No Responses to “Chest-Pain Case Reminds Us of the Importance of Clinical Decision Tools”