
The Centers for Medicare and Medicaid Services (CMS) has released two long awaited proposed rules: the 2020 Physician Fee Schedule (PFS) and the 2020 Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Center (ASC) Payment System. ACEP provided extensive commentary on these proposed rules, and CMS is expected to finalize these provisions by early November 2019. Overall, CMS has recognized that emergency medicine is providing higher-intensity care and, as a result, our work relative value units (RVUs) will be increasing.
Explore This Issue
ACEP Now: Vol 38 – No 10 – October 2019You can read ACEP-submitted commentary on the proposed PFS rule.
2020 Conversion Factor Increase
For 2020, CMS proposes a Medicare PFS conversion factor of $36.0896 representing a small increase from the 2019 conversion factor of $36.0391. Note that the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) provided 0.5% base updates to the conversion factor through 2019. Those base updates have now expired, leading to this relatively smaller increase.
2020 RVUs Increase for ED E/M Services
Each year, RVU values for physician services are updated. This year, CMS had concerns that the emergency department evaluation and management (E/M) Current Procedural Terminology (CPT) codes were undervalued and requested that the American Medical Association’s Relative Value Update Committee (RUC) perform a survey and revalue the work RVUs associated with the relevant codes.
“In the CY 2018 PFS final rule, we finalized a proposal to nominate CPT codes 99281–99285 as potentially misvalued based on information suggesting that the work RVUs for emergency department visits may not appropriately reflect the full resources involved in furnishing these services (FR 82 53018).”—2019 Physician Proposed Rule, page 420
ACEP undertook an extensive survey process and mounted compelling arguments describing the increased complexity of the patients we treat every day in the nation’s emergency departments. (Read more about ACEP’s efforts to increase emergency physicians’ reimbursement rates at ACEP4U.) In good news for emergency medicine, CMS has proposed to revalue the codes based on the RUC recommended work values (see Table 1). (To read behind-the-scenes information about how our ACEP volunteers and staff formed the winning arguments, read our previous ACEP4U article from the September 2019 issue.)
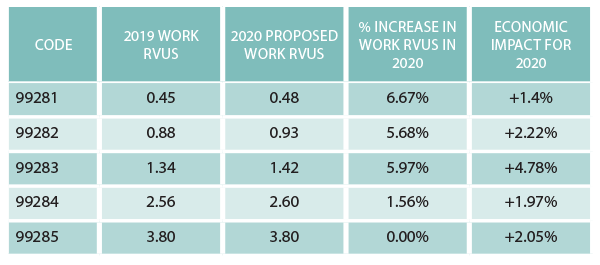
Table 1: 2020 Proposed Increases to ED Work RVUs
A more detailed fact sheet on the 2020 PFS payment proposals.
Merit-Based Incentive Payment System
The Merit-Based Incentive Payment System (MIPS) is a payment mechanism that provides for annual reimbursement adjustments related to CMS quality program requirements in four categories: quality, cost, promoting interoperability, and clinical practice improvement activities. For the 2020 performance year (affecting 2022 payments), the relevant MIPS categories for typical emergency medicine groups will include (see Figure 1):
- Quality: 65 percent
- Cost: 20 percent
- Improvement activities: 15 percent

Figure 1: 2020 MIPS Category Weighting for Typical ED Providers
In the proposed rules, CMS also advances some significant changes to MIPS, including:
MIPS Performance Thresholds Increasing, Making It Harder to Avoid a Penalty
- CMS proposes to increase the MIPS performance threshold, which is the minimum number of points needed to avoid a negative payment adjustment, from 30 points in 2019 to 45 points in 2020 and 60 points in 2021 (see Figures 2 and 3).
- CMS also proposes to increase the exceptional performance threshold (which allows for extra bonus dollars) from 75 points in 2019 to 80 points in 2020 and 85 points in 2021.
- CMS proposes to increase the quality measure data completeness reporting requirement from 60 percent to 70 percent of applicable patients.
Quality Category Goes Down, Cost Goes Up
- CMS proposes to reduce the weight of the quality category for general medical providers from 50 percent to 40 percent in 2020, 35 percent in 2021, and 30 percent in 2022 while correspondingly increasing the weight and impact of the cost category.
- For each individual quality measure, a provider’s raw percentage of meeting the measure’s requirements is benchmarked against the universe of providers reporting that measure to yield a decile score. Each decile is then converted to a MIPS quality point score on a scale of 1–10. Your “quality points” are then added to your total MIPS score based on the weighting of the quality category for your reporting entity.
The cost category is calculated based on 10 measures:
- Total per capita costs for all attributed beneficiaries measure
- Medicare spending per beneficiary measure
- Elective outpatient percutaneous coronary intervention
- Knee arthroplasty
- Revascularization for lower extremity chronic critical limb ischemia
- Routine cataract removal with intraocular lens implantation
- Screening/surveillance colonoscopy
- Intracranial hemorrhage or cerebral infarction
- Simple pneumonia with hospitalization
- ST-elevation myocardial infarction with percutaneous coronary intervention
CMS Proposes Multiple Changes to Emergency Medicine–Focused Quality Measures
- To remove the following measures from the emergency medicine specialty set, meaning that CMS no longer views these as relevant to emergency physicians: #91: acute otitis externa: topical therapy; and #255: Rh immunoglobulin (Rhogam) for Rh-negative pregnant women at risk of fetal blood exposure.
- To remove the claims-based version of measure #415: emergency department utilization of CT for minor blunt head trauma for patients aged 18 years and older from MIPS due to topped-out status but to maintain the measure for registry reporting.
- To remove emergency department patients from inclusion in measure #326: atrial fibrillation and atrial flutter: chronic anticoagulation therapy.
CEDR Can Help
The penalty for not meeting MIPS requirements in 2020 will be 9 percent for typical ED groups. ACEP Clinical Emergency Data Registry (CEDR) is available as an EM-specific reporting mechanism to take care of your MIPS reporting requirements. Learn more.
MIPS Value Pathways Framework
CMS has published a brand-new term, the “MIPS Value Pathways Framework” (MVPs). As part of the proposed rules, CMS is seeking feedback on its new MVPs, which aims to move MIPS toward a new set of measures that are more clinically relevant for each provider.
CMS proposes that a clinician or group has the choice to opt into an MVP associated with their specialty or opt into a clinical condition. Providers would be reporting on the same measures and activities as other clinicians and groups in the MVP that the provider has opted into. Each MVP “track” would connect measures and activities across the various MIPS performance categories and could rely on a mix of specialty-specific measures as well as population-based administrative claims-based measures automatically calculated by CMS. MVPs would also include more robust and timely performance feedback to better prepare clinicians for transitioning to risk-based alternative payment models. MVPs could begin to apply as early as the 2021 performance year.
A more detailed fact sheet on proposed changes to the quality payment program can be found here.
Hospital Price Transparency
As part of the proposed OPPS rule, CMS published a series of proposals that collectively aim to increase the transparency of hospital charges. Notably, CMS is proposing requirements that would force hospitals to make their private-payer negotiated (contracted) rates (for “shoppable” services) available to the public.
Hospital Clinic, Emergency Department, and Critical Care Payments
CMS proposed no major changes for hospital-based clinics and emergency department facility payments as well as facility critical care services and trauma activation services. The policies for these services would also remain generally unchanged.
A more detailed fact sheet regarding both the payment and quality proposals in the OPPS rule can be found here.
Need More Help?
Resources for these and other topics can be found on the reimbursement section of the ACEP website, www.acep.org/administration/reimbursement. ACEP Director of Reimbursement David McKenzie, CAE, can field questions at 800-708-1822, ext. 3233. Finally, ACEP offers well-attended and highly recommended coding and reimbursement educational conferences annually, with the next conference scheduled for Jan. 27–31 in Austin, Texas. Visit www.acep.org/rc for details.
Dr. Granovsky is president of LogixHealth, an ED coding and billing company, and currently serves as the course director of ACEP’s Coding and Reimbursement courses. He may be reached at mgranovsky@logixhealth.com.
Mr. McKenzie is ACEP director of reimbursement.
Pages: 1 2 3 | Multi-Page





No Responses to “CMS Proposed Rule Includes 2020 Emergency Physician Compensation Increase”