
Lately, the topic of competency of advanced practice providers (APPs), also known as physician assistants (PAs) and nurse practitioners (NPs), has come up frequently within hospitals and large health care organizations. These groups have been hiring more new APP graduates and want to know how long it will take for them to get up to speed within the institution. Additionally, it is a point of contention within emergency medicine, with some EM groups refusing to take new graduates until they demonstrate the necessary knowledge and skills—a Catch-22 if I’ve heard one. Don’t get me wrong! This is an important issue within a strongly procedure-based specialty in which clinical acumen must remain high. Emergency medicine is also a specialty among APPs that is highly sought (see Figure 1). Nonetheless, APPs seeking to work in emergency medicine must demonstrate they have advanced knowledge and experience in emergency medicine above and beyond that expected of entry-level APPs working in a generalist practice.
Explore This Issue
ACEP Now: Vol 34 – No 02 – February 2015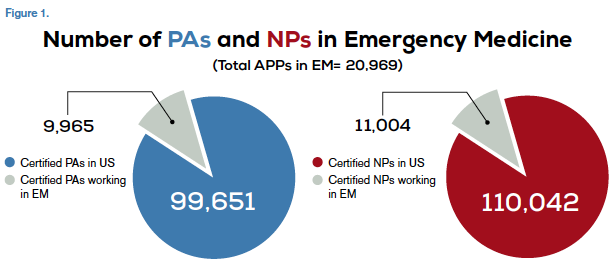
Sources
http://www.aapa
http://kff.org/other/state-indicator/total-nurse-practitioners/>
http://bhpr.hrsa.gov/healthworkforce/supplydemand/usworkforce/chartbook/chartbookpart1.pdf
Competence is defined not so much as “how long” but rather the achievement of the skill sets needed to practice in an ED. It is a narrow, specific question rather than a broad, philosophical one.
While there are a number of definitions of clinical competency, I prefer Norman’s definition of professional competence: “The habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served. Competence builds on a foundation of basic clinical skills, scientific knowledge, and moral development.”1
He goes on to say that competence has multiple functions: cognitive (using acquired knowledge to solve real-life problems), integrative (using biomedical and psychosocial data in clinical reasoning), relational (communicating effectively with patients and colleagues), and affective/moral (the willingness, patience, and emotional awareness to use these skills judiciously and humanely). I was struck by a final comment that competence is “developmental, impermanent, and context-dependent.”1 Competence is certainly developmental in the context of lifelong learning. If it is indeed impermanent (temporary, transient, transitory, passing, fleeting), then it must be evaluated frequently. There is no argument that it is context-dependent, whether by level of care, specialty knowledge required, or institution.
Clearly, competence is complex. While the PA and NP professions have developed and published a list of specific skills necessary to be considered competent, which mirror and parallel those of our physician colleagues, the question becomes, “How do we actually demonstrate them?”
Pages: 1 2 3 4 | Single Page





One Response to “Competency Measurement Approach for Advanced Practice Providers in Emergency Medicine”
February 16, 2015
Gerry KeenanA timely explanation!We can only hope it guides reasoned decision making.