Annually, more than 300,000 adults older than age 65 are hospitalized for hip fractures, which frequently result from ground-level falls.1 Emergency medical professionals are tasked with providing care and analgesia for patients with femoral neck fractures. Monotherapy with intravenous opioids can often lead to undesired complications (eg, delirium, diminished respiratory drive, and nausea).2–4 The ultrasound-guided femoral nerve block (USGFNB) and ultrasound-guided fascia iliaca compartment block (USGFICB) offer improved pain control as well as reduced side effects in comparison with monotherapy with intravenous opioids.4,5
Explore This Issue
ACEP Now: Vol 37 – No 01 – January 2018Even though USGFNB has been described extensively in the emergency medicine literature, its use has not become commonplace. The perceived technical difficulty of the USGFNB may contribute to its current underutilization in acute traumatic femoral neck fractures.6,7 However, the USGFICB may be a potentially easier technique for the novice sonographer. Evidence supporting this theory includes the technique’s proven efficacy in the hands of a variety of clinicians, including resident physicians, nurses, and paramedics.8–10
Anatomy
Sensory innervation of the femoral neck is primarily provided by articular branches of the femoral nerve with minor contributions from the obturator nerve and the superior and inferior gluteal nerves. The femoral nerve (L2–L4) and the obturator nerve (L2–L4) both transverse a compartment that spans the lower abdomen and anterior thigh and is confined anteriorly by the fascia iliaca (ie, fascia iliaca compartment). While both the femoral and obturator nerves course through the same compartment, deposition of large volumes of local anesthesia under the fascia iliaca (as with USGFICB) seldom successfully blocks the obturator nerve.11 That said, available evidence also suggests that the obturator nerve minimally contributes to distal sensory innervation.12
To perform a USGFICB, two approaches exist. Both have the goal of injecting local anesthetic into the compartment lateral to the femoral nerve, which lies lateral and adjacent to the vascular bundle (see Figure 1). The two approaches are the infrainguinal (see Figure 2A) and the suprainguinal (see Figure 2B).
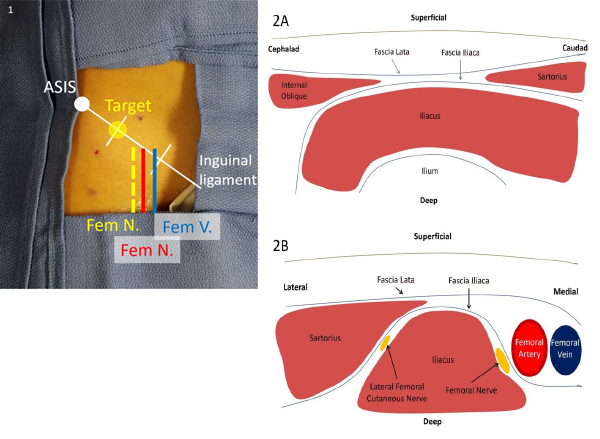
Figure 1. The inguinal ligament may be divided into thirds, with the target site for injection being the lateral one-third mark. This lies lateral to the femoral nerve and vasculature.
Figure 2. A: In the infrainguinal approach, the fascia lata and fascia iliaca form a “bow tie” when overlapping between the sartorius caudad and internal oblique cephalad, with underlying iliacus muscle spanning over the ilium. B: In the suprainguinal approach, the sartorius overlies the iliacus muscle on its lateral border, with the fascia iliaca separating the two muscles. The femoral nerve and vascular bundle lie medial to the iliacus muscle, and the lateral femoral cutaneous nerve lies between the muscle bodies.
Supplies
- High-frequency linear transducer (6–10 MHz) with sterile lubricant
- 0.5% ropivacaine (5 mg/mL): dilute 30 mL 0.5% ropivacaine into 30 mL 0.9% normal saline
- Max dose is commonly considered 3 mg/kg.
- Ropivacaine is the preferred local anesthetic due to its long-acting duration with a greater safety profile than bupivacaine.13
- Mixing of local anesthetics is not currently advised due to less predictable onset, duration, and potency.13
- 22-gauge blunt-tipped echogenic needle (Whitacre and Sprotte needles are blunt-tipped needles, which provide better tactile feedback when “popping through” the fascia lata and fascia iliaca.)
- IV tubing connected to a 30 or 60 mL syringe
- Chlorhexidine scrub or alcohol prep sponge
- Local anesthetic for cutaneous anesthesia (eg, 12% lidocaine without epinephrine)
- Personal protection equipment including sterile gloves
- Second provider present for assistance
- Airway supplies and 20% lipid emulsion available
With the above supplies prepared and on standby, perform a preprocedure scan to determine the patient’s specific anatomy. Prepare the selected injection site with chlorhexidine or isopropyl alcohol. A skin marker may help maintain proper orientation to the injection site. Next, flush the premixed 30 mL of ropivacaine and normal saline through the line and echogenic needle.
Preprocedural Nerve Block
As with any proximal nerve block, several steps should be addressed prior to beginning the procedure. First, a thorough neurological exam should be performed. Discussion with the orthopedic service at your institution is recommended before US-guided nerve blocks for hip fractures are performed. A detailed lower extremity neurovascular examination must be performed and documented. Patients should be placed on continuous cardiac monitoring and pulse oximetry to monitor for local anesthetic systemic toxicity. The risk of local anesthetic systemic toxicity (both neurological and cardiovascular) is highest in cases of unintentional intravascular injection. In addition to supportive, anti-seizure, and cardiac resuscitation measures, early administration of lipid emulsion antidote is recommended with prolonged seizure and/or any cardiac arrhythmia. Providers should be aware of Intralipid (20% lipid emulsion) availability and dosing prior to injecting large volumes of local anesthetic.14 Lipid emulsion effectively creates a “lipid sink” where the local anesthetic is soluble with, and bound by, the lipid molecules.
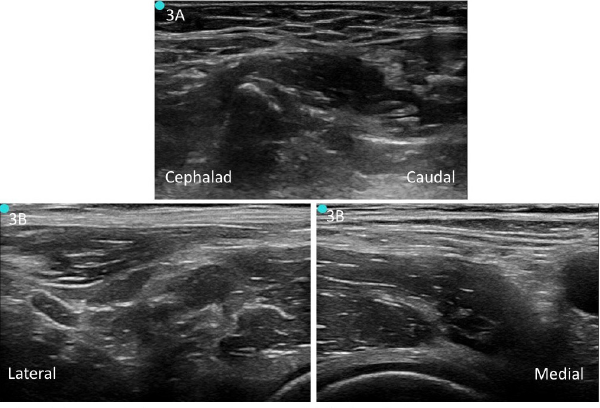
Figure 3. A: Unlabeled preprocedure scan of infrainguinal approach. B: Unlabeled preprocedure scan of suprainguinal approach.
To perform a USGFICB, place the patient supine (slight Trendelenburg position if tolerated) and place the US system contralateral to the extremity being blocked. This will allow the clinician to have a clear view of the US screen when performing the block. Perform a preprocedure scan of the anatomy with a linear transducer (6–10MHz) (see Figures 3A and 3B). If aberrant anatomy distorts landmarks and the proper fascial layers cannot be properly identified, consider aborting the procedure. Clean the target needle entry site and probe and make a small skin wheal with 1–2% lidocaine. Clean the area with a chlorhexidine scrub.
Nerve Block Procedures
Infrainguinal USGFICB. Place your US transducer perpendicular to the inguinal ligament at a third of the distance between the anterior superior iliac spine and pubic symphysis (see Figure 4A), with the transducer indicator oriented cephalad. After visualizing the pulsating femoral artery, locate the hyperechoic femoral nerve immediately lateral. Slide the transducer laterally to identify the sartorius muscle caudad and iliacus muscle cephalad, with the fascia lata and fascia iliaca forming a “bow tie” over the iliacus muscle. Place a skin wheal just caudal to the transducer, marking the location that the block needle will enter.
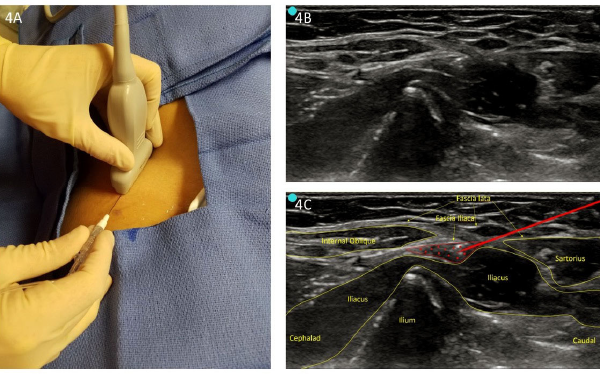
Figure 4. A: Infrainguinal approach (perpendicular to inguinal ligament). B: Unlabeled infrainguinal preprocedure scan. C: Labeled image with infiltration.
Insert the needle in-plane to provide a long view of the needle. Guide the needle below the inguinal ligament and through the fascia lata and fascia iliaca at the center of the “bow tie.” When using a blunt-tipped needle, a palpable “pop” may be felt when puncturing these two fascial layers. Once through the fascia iliaca, aspirate and then inject 2–3 mL of local anesthetic to confirm needle placement (see Figures 4B and 4C). Hydro-dissection of the fascia iliaca from the iliacus muscle demonstrates correct placement. Gently continue to hydro-dissect with 30–60 mL of local anesthetic in 5 mL increments with gentle aspirations between injections to ensure avoidance of inadvertent vascular puncture.
Suprainguinal USGFICB. Place the transducer just superior and parallel to the inguinal ligament (see Figure 5A). Slide the transducer medially to visualize common sonoanatomy (eg, femoral vein, femoral artery, and femoral nerve). Slowly move the transducer laterally to visualize the sartorius muscle overlying the iliacus muscle. Place a skin wheal just lateral to the transducer, marking the location that the block needle will enter. Insert the needle in-plane from lateral to medial, visualizing the needle in long axis. The needle should course through the sartorius muscle or just superficial and sit between the iliacus muscle and fascia iliaca, lateral to the neurovascular bundle.15 Once deep to the fascia iliaca, aspirate and inject 2–3 mL of local anesthetic to confirm needle placement (see Figures 5B and 5C). If there is separation between the fascia iliaca and iliacus muscle, gently hydro-dissect with 30–60 mL of local anesthetic in 5 mlL increments with gentle aspirations between injections to ensure lack of inadvertent vascular puncture.
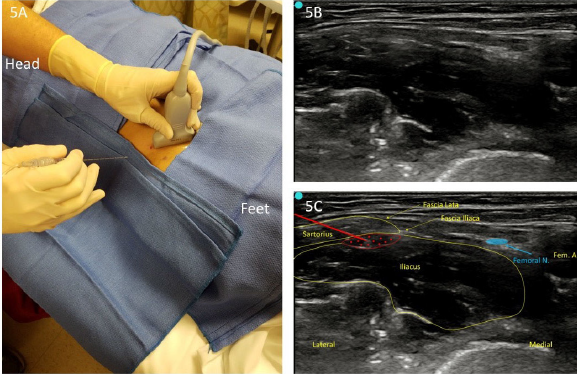
Figure 5. A: Suprainguinal approach (lateral to medial). B: Unlabeled infiltration view. C: Labeled infiltration view.
Summary
A multimodal pain management approach that incorporates USGFICB for patients with acute femoral neck fractures has been demonstrated to reduce the reliance on opioids.16 Specifically in the elderly patient, this bedside intervention can reduce unwanted side effects commonly seen with opioids while offering significant pain control. USGFICB may be an ideal option for sonographers who are less comfortable performing USGFNB.
Dr. LaJeunesse is a captain in the U.S. Army Medical Corps and a second year EM resident at Madigan Army Medical Center (MAMC) in Tacoma, Washington. Mr. Cronin is a major in the U.S. Army Medical Specialist Corps and program director and assistant professor of the U.S. Army-Baylor University emergency medicine PA residency at MAMC. Dr. Takahashi is a captain in the U.S. Army Medical Corps, a family medicine physician, and an emergency ultrasound fellow at MAMC. Mr. Knudsen is a captain in the U.S. Army Medical Specialist Corps and an emergency medicine resident and doctoral candidate at MAMC. Dr. Nagdev is director of emergency ultrasound at Highland Hospital, Alameda Health System, in Oakland, California.
References
- Hip fractures among older adults. Centers for Disease Control and Prevention website. Accessed Dec. 14, 2017.
- Mutty CE, Jensen EJ, Manka MA Jr, et al. Femoral nerve block for diaphyseal and distal femoral fractures in the emergency department. J Bone Joint Surg Am. 2008;90(Suppl 2 Pt 2):218-226.
- Mouzopoulos G, Vasiliadis G, Lasanianos N, et al. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol. 2009;10(3):127-133.
- Foss NB, Kristensen BB, Bundgaard M, et al. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007;106(4):773-778.
- Odor Pm, Chis Ster I, Wilkinson I, et al. Effect of admission fascia iliaca compartment blocks on post-operative abbreviated mental test scores in elderly fractured neck of femur patients: a retrospective cohort study. BMC Anesthesiol. 2017;17(1):2.
- Grabinsky A, Sharar SR. Regional anesthesia for acute traumatic injuries in the emergency room. Expert Rev Neurother. 2009;9(11):1677-1690.
- Reavley P, Montgomery AA, Smith JE, et al. Randomised trial of the fascia iliaca block versus the ‘3-in-1’ block for femoral neck fractures in the emergency department. Emerg Med J. 2015;32(9);685-689.
- Hogh A, Dremstrup L, Jensen SS, et al. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies Trauma Limb Reconstr. 2008;3(2):65-70.
- Dochez E, van Geffen GJ, Bruhn J, et al. Prehospital administered fascia iliaca compartment block by emergency medical service nurses, a feasibility study. Scand J Trauma Resusc Emerg Med. 2014;22:38.
- McRae PJ, Bendall JC, Madigan V, et al. Paramedic-performed fascia iliaca compartment block for femoral fractures: a controlled trial. Journal Emerg Med. 2015;48(5):581-589.
- Swenson JD, Davis JJ, Stream JO, et al. Local anesthetic injection deep to the fascia iliaca at the level of the inguinal ligament: the pattern of distribution and effects on the obturator nerve. J Clin Anesth. 2015;27:652-657,
- Kardash K, Hickey D, Tessler MJ, et al. Obturator versus femoral nerve block for analgesia after total knee arthroplasty. Anesth Analg. 2007;105(3):853-858.
- Gadsden J. Local anesthetics: clinical pharmacology and rational selection. The New York School of Regional Anesthesia website. Accessed Dec. 15, 2017.
- Wolfe JW, Butterworth JF. Local anesthetic systemic toxicity: update on mechanisms and treatment. Curr Opin Anaesthesiol. 2011;24:561-566.
- Hebbard P, Ivanusic J, Sha S. Ultrasound-guided supra-inguinal fascia iliaca block: a cadaveric evaluation of a novel approach. Anaesthesia. 2011;66(4):300-305.
- Groot L, Dijksman LM, Simons MP, et al. Single fascia iliaca compartment block is safe and effective for emergency pain relief in hip-fracture patients. West J Emerg Med. 2015;16(7):1188-1193.
Pages: 1 2 3 4 | Multi-Page





5 Responses to “Control Hip Fracture Pain Without Opioids Using Ultrasound-Guided Fascia Iliaca Compartment Block”
January 27, 2018
Ron BraceThe diagram, first color coded one showing locations of Fem nerve vein and artery is seriously mislabeled and a correction need be done; Femoral Vein is in wrong place, as is the Femoral artery – and the fem artery is mislabeled
I am sure by now a thousand people have written about it!
https://www.acepnow.com/wp-content/uploads/2018/01/ACEP_0118_pg20a.png
January 28, 2018
Robert A.Great article. I think Figure 1 is mislabeled: Femoral artery is mislabeled as “Fem V.” and Femoral vein mislabeled as “Fem N. (red)”.
February 5, 2018
HosamIn illustration, I think that order of structures are not proper.it is vien artery nerve from medial to lateral
February 5, 2018
MikeHi, picture 1 seems to have some errors. There are two structures markes Fem N, one of them in red which is likely supposed to be the Fem Artery. If that structure is supposed to the fem artery it is incorrectly positioned medial to the femoral vein when it should be lateral
February 5, 2018
Dawn Antoline-WangThank you to everyone who pointed out the error in Figure 1. The image has been corrected.