Case: A 49-year-old man with no past medical history presents to the ED with palpitations for five days. He feels tired and a little short of breath but has no chest pain. His vital signs are normal except for a heart rate of 142 beats per minute (bpm). You palpate his pulse and find it irregularly irregular. An ECG confirms rapid atrial fibrillation.
Explore This Issue
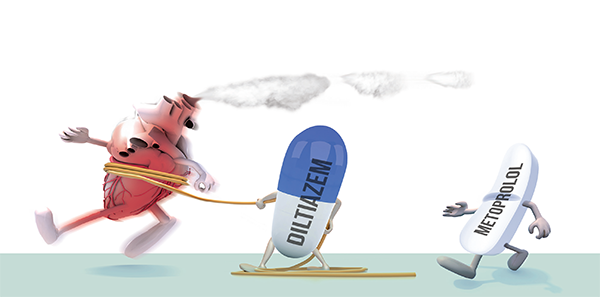
ACEP Now: Vol 35 – No 01 – January 2016Question: In patients with rapid atrial fibrillation, what medication will obtain rate control faster: a beta blocker or a calcium channel blocker?
Background: Atrial fibrillation is a common presentation to the ED, with atrial flutter being less common. There has been controversy as to whether rhythm control is better than rate control for these dysrhythmias. An aggressive rhythm control protocol demonstrating efficacy and safety for early-onset atrial fibrillation or flutter (AFF) has been published.1
Rhythm control would not be an option in this case because this man’s symptoms have been present for five days. Rate control is the treatment of choice for stable patients with atrial fibrillation >48 hours or an unknown time of onset with a rapid ventricular response.2 However, there is limited evidence on whether beta blockers or calcium channel blockers are better for achieving rate control.3
There has been controversy as to whether rhythm control is better than rate control for these dysrhythmias.
Relevant Article: Fromm C, Suau SJ, Cohen V, et al. Diltiazem vs. metoprolol in the management of atrial fibrillation or flutter with rapid ventricular rate in the emergency department. J Emerg Med. 2015;49(2):175-182.
- Population: Adult patients >18 years old presenting with atrial fibrillation or atrial flutter. There were many exclusions listed in the paper.
- Intervention: Diltiazem 0.25 mg/kg (max dose of 30 mg) or metoprolol 0.15 mg/kg (max dose of 10 mg) IV.
- Comparison: As above.
- Outcome:
- Primary: Heart rate <100 bpm within 30 minutes.
- Safety: Heart rate <60 bpm and systolic blood pressure <90 mmHg.
Authors’ Conclusions: “Diltiazem was more effective in achieving rate control in ED patients with AFF and did so with no increased incidence of adverse effects.”
Key Results: There were 28 patients randomized to the metoprolol group and 24 in the diltiazem group. About two-thirds of the patients were new-onset atrial fibrillation. The mean age was 66 years, and 47 percent were men.
Primary Outcome: HR<100 bpm at 30 minutes 96 percent diltiazem vs. 46 percent metoprolol (number needed to treat=2)
No difference was noted between the groups in terms of bradycardia or hypotension.
EBM Commentary:
- Convenience sample: This was a convenience sample of patients, not consecutive patients, presenting to the ED with rapid atrial fibrillation, which could introduce selection bias.
- Stopped early: The trial was stopped early after recruiting only 54 of the 200 patients required based on their power calculation for a noninferiority trial. There are differences between noninferiority, superiority, and equivalence trials.4 Concerns have been raised in the literature about the ethics and problems of stopping trials early.5,6
- Medication dose: The diltiazem was dosed at 0.25 mg/kg (max of 30 mg), and the metoprolol was given at 0.15 mg/kg (max of 10 mg). This may not be an equivalent comparison with underdosing of the metoprolol.
- Physician-oriented outcome: The primary outcome of heart rate <100 bpm at 30 minutes may have been more of a physician-oriented outcome rather than a patient-oriented outcome. Physicians’ priorities are to get the heart rate down and disposition the patient. However, the priorities of the patients could have been different and were not explored in this study.
- Single center: This was a single-center study of an inner-city population. A multicenter study with a diverse population would have made the results more robust.
Bottom Line: Despite the limitations of the study, it appears that diltiazem will achieve more rapid rate control in patients with atrial fibrillation than metoprolol.
Case Resolution: A slow push of diltiazem 0.25 mg/kg was given, and his rate dropped to 89 bpm. The patient was started on oral diltiazem to continue his rate control. His CHA2DS2-VASc score was found to be very low risk for stroke. Therefore, he was started on aspirin alone and discharged home with follow-up with a cardiologist in a couple of days.
Thank you to Dr. Anand Swaminathan, assistant residency director of the NYU/Bellevue Emergency Medicine residency program (CoreEM), for his help with this review.
Remember to be skeptical of anything you learn, even if you heard it on the Skeptics’ Guide to Emergency Medicine.
 Dr. Milne is chief of emergency medicine and chief of staff at South Huron Hospital, Ontario, Canada. He is on the Best Evidence in Emergency Medicine faculty and is creator of the knowledge translation project the Skeptics’ Guide to Emergency Medicine.
Dr. Milne is chief of emergency medicine and chief of staff at South Huron Hospital, Ontario, Canada. He is on the Best Evidence in Emergency Medicine faculty and is creator of the knowledge translation project the Skeptics’ Guide to Emergency Medicine.
References
- Stiell IG, Clement CM, Perry JJ, et al. Association of the Ottawa Aggressive Protocol with rapid discharge of emergency department patients with recent-onset atrial fibrillation or flutter. CJEM. 2010;12(3):181-191.
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. J Am Coll Cardiol. 2014;64(21):2246-2280.
- Demircan C, Cikriklar HI, Engindeniz Z, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005;22(6):411-414.
- Mulla SM, Scott IA, Jackevicius CA, et al. How to use a noninferiority trial: users’ guides to the medical literature. JAMA. 2012;308(24):2605-2611.
- Montori VM, Devereaux PJ, Adhikari NK, et al. Randomized trials stopped early for benefit: a systematic review. JAMA. 2005;294(17)2203-2209.
- Mueller PS, Montori VM, Bassler D, et al. Ethical issues in stopping randomized trials early because of apparent benefit. Ann Intern Med. 2007;146(12)878-881.
Pages: 1 2 3 | Multi-Page

 ACEP Now features one article each issue related to an ACEP eCME CME activity.
ACEP Now features one article each issue related to an ACEP eCME CME activity.




2 Responses to “Diltiazem Achieves More Rapid Rate Control in Atrial Fibrillation than Metoprolol”
January 24, 2016
HCAnyone adding IV magnesium to IV Cardizem & obtaining higher success of spontaneous conversion?
December 26, 2016
FMarkMoore/MDIs it safer to do a TE echo first to determine clots in non anticoagulated patients off the street?